THURSDAY, Aug. 18 (HealthDay News) — Many doctors continue to recommend annual screening for cervical cancer, even though current guidelines say some women can wait much longer between tests.
Those are the findings of a new study by Katherine Roland, a behavioral scientist at the U.S. Centers for Disease Control and Prevention.
“These findings are in conflict with the guidelines,” Roland said.
The downsides of too-frequent testing, she said, include excess costs, pain and the inconvenience of having to visit the doctor more often than necessary.
For the study, published online Aug. 18 in the American Journal of Obstetrics & Gynecology, Roland evaluated data from two national surveys from 2006 and found that the majority of health care providers still advised annual screenings, even when test results and a woman’s history suggested it wasn’t needed.
Her team also reviewed responses from 376 private office-based health care providers and 216 providers from hospitals and outpatient facilities.
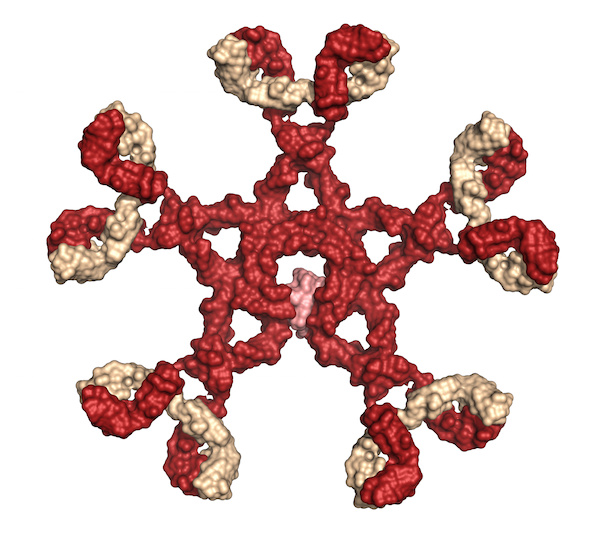
Under cervical cancer screening guidelines issued by the American Cancer Society in 2002 and the American College of Obstetricians and Gynecologists in 2003, women aged 30 or older should have both a Pap test, also known as a Pap smear, and a human papillomavirus (HPV) test, also called an HPV co-test. HPV is the most common sexually transmitted infection, and certain types of HPV can cause cervical cancer.
If the results of both tests are normal, a woman can wait three years for her next Pap test, which looks for signs of cancer in cells from a woman’s cervix.
Roland presented three scenarios to the doctors and other health care providers, each involving a woman between 30 and 60 years old with a current normal Pap test. In one vignette, she had no current HPV test result and a history of two normal Pap tests. In a second, she had a current negative HPV test and two consecutive normal Pap tests. In the third, she had a current negative HPV test and no Pap history besides the current one.
While all three scenarios would warrant recommending an interval of three years, most of the doctors and others who performed the tests still would recommend yearly screening, the investigators reported.
“We found that only half the providers are using the HPV co-test,” Roland said. She couldn’t explain why that is so, or why they continue to order annual screens even if they perform both tests as advised.
Among the study limitations, however, is that office staff often answered the questions, which may have affected the accuracy, the study authors said.
A conventional Pap test costs about $14, Roland said, and a liquid-based cytology type test is about $28. The cost of the HPV test varies, she noted.
The findings puzzle Dr. Elizabeth Poynor, a gynecologic oncologist and pelvic surgeon at Lenox Hill Hospital in New York City. “What struck me was the slow nature of the physicians to accept the new guidelines,” Poynor said.
But, she pointed out that the HPV co-test was new when the data was collected in 2006. Today, more doctors could be using the test and extending the interval between screenings. Maybe doctors need to get used to the guidelines, to develop a comfort level with the less frequent screening, she said.
The guidelines make sense, Poynor added. “When you combine a negative HPV and a negative Pap, the false negative rate goes down to a very low level,” she said.
Women can take this information to their doctors and “use it as a point for dialogue or discussion,” Poynor suggested.
However, it’s crucial to realize that the screening guidelines apply only to women 30 to 60 who are healthy, Poynor stressed. They don’t apply to women with certain medical risk factors, such as exposure to the prescription drug DES (diethylstilbestrol), which has been linked to cancer.
And, it’s important to tell women they still need an annual pelvic exam, Poynor said.
More information
To learn more about Pap testing, visit WomensHealth.gov.