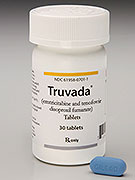
MONDAY, July 16 (HealthDay News) — For the first time, the U.S. Food and Drug Administration has approved the use of a pill to help prevent HIV infection in uninfected, high-risk people.
“[The] FDA is approving Truvada, taken daily for pre-exposure prophylaxis, or PReP, in combination with safer sex practices, to reduce the risk of sexually acquired HIV infection in at-risk adults,” Dr. Debra Birnkrant, director of the division of antiviral products at the FDA’s Center for Drug Evaluation and Research, said during a Monday news conference. “This is the first drug approved for PReP in combination with safer sex practices to reduce the risk of sexually acquired HIV infection.”
The safer sex practices recommended by the FDA include HIV testing every three months, strict adherence to recommended dosing and counseling.
“Truvada alone should not be used to prevent HIV infection,” Birnkrant stressed, adding that studies have shown that condom use increased in people using Truvada while the rate of other sexually transmitted diseases (STDs) either remained stable or also decreased.
Birnkrant added that she anticipated that Truvada, along with accompanying safer sex messages, will help achieve the federal government’s National HIV/AIDS Strategy goal of reducing the number of new infections in the United States by 25 percent by 2015.
The decision comes two months to the day after an FDA advisory panel voted for approval of Truvada for use by healthy, at-risk individuals, including gay and bisexual men and heterosexual couples with one HIV-infected person.
It also comes before the biennial International AIDS Conference, slated to start Sunday in Washington, D.C.
Truvada has been available since 2004 to treat people already infected with HIV.
However, some experts believe that there are potential drawbacks to using the medication as a way to try to prevent HIV infection. Truvada — which combines two HIV-fighting drugs, tenofovir (Viread) and emtricitabine (Emtriva) — is very expensive and may cause side effects. And although doctors can already prescribe it to people trying to avoid HIV infection, some critics contend that it’s too early to officially allow it to be promoted for that use.
On the other hand, those who support marketing the drug as a preventive agent say it can help high-risk people avoid the disease, especially if they don’t use condoms or if they want an added layer of protection.
“I don’t see it as a panacea, but it’s an option, and that’s important,” Dr. Kenneth Mayer, an AIDS specialist and medical research director of The Fenway Institute at Fenway Health in Boston, said in May when the advisory panel endorsed the idea. “Some people won’t use a condom, but will say, ‘If you give me another option, I’ll use that.'”
Truvada works to combat HIV from replicating in the body’s cells. Mayer explained that in someone who is not yet infected but is exposed to HIV, the drug may prevent the virus from reproducing even if it has already invaded cells. As a result, he said, “the virus cannot start turning the newly exposed person’s body into a ‘factory’ to produce more HIV particles.”
A study published in 2010 in the New England Journal of Medicine found that Truvada cut the risk of HIV infection by almost 44 percent in those at highest risk for contracting the virus, namely sexually active gay and bisexual men. The risk reduction climbed to nearly 73 percent among study participants who took the pill 90 percent of the time, the researchers added.
A. David Paltiel, a professor at Yale University School of Medicine, said his research has shown that the use of preventive drug treatments should reduce the risk of infection overall. Still, he said, it’s unknown if “people [would] take more chances because they feel protected by a ‘chemical condom.'”
Mayer, who has conducted research on the drug, said that allowing the marketing will probably lead to an increase in its usage for prevention. But, “this is not a one-time, end-of-the-problem approach like a shot of penicillin to treat an infection like syphilis,” he said. “Also, it involves someone perceiving that he or she is at risk, or a provider being comfortable enough to ask about a person’s risk. We know that a lot of health providers don’t like to talk to their patients about sex.”
Truvada, which is manufactured by Gilead Sciences, can also cause a long list of side effects, including gastrointestinal, bone and kidney problems. In an FDA statement released Monday, the agency said that “while effects observed in clinical trials were mild and reversible with discontinuation of the medication, people with a history of bone or kidney ailments should be regularly monitored to ensure their continued health.”
The FDA approval comes with a REMS (Risk Evaluation and Mitigation Strategy) plan, which includes regular testing, health care professional education, risk-mitigating measures, voluntary training and education for potential prescribers and a medication guide and safety brochure.
People who take Truvada should also be tested for hepatitis B, the agency said, “because worsening of hepatitis B infections has been reported in those who have both HIV-1 and hepatitis B when treatment with Truvada was stopped.”
The drug is also costly, with prices in the United States tagged at about $26 a day, or $10,000 a year. Still, a study released this year found the drug would be cost-effective if used extensively by gay and bisexual men at high risk of becoming infected.
More information
Find out more about HIV/AIDS at the U.S. National Library of Medicine.