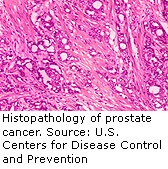
TUESDAY, May 4 (HealthDay News) — When the U.S. Food and Drug Administration announced Monday it was investigating possible links between widely used hormonal prostate cancer drugs and an slight rise in risk for diabetes and heart disease, thousands of men who rely on these drugs to extend their lives were left wondering what to do next.
According to experts, the main advice to those men at the moment is to keep taking the drugs, but use them with caution.
The FDA says it will review a widely used class of prostate cancer drugs called gonadotropin-releasing hormone (GnRH) agonists. These include medications such as Eligard, Lupron, Synarel, Trelstar, Vantas, Viadur, Zoladex and several generic products.
All of these drugs suppress the production of testosterone, a hormone thought to help spur the growth of prostate cancer. Hormone-based therapy is not a cure for prostate cancer, because tumors can eventually become resistant, but it can extend survival.
“Clearly these drugs are needed for the treatment of prostate cancer,” stressed prostate cancer expert Dr. Mark Soloway, chair of urology at the University of Miami Miller School of Medicine.
“Lowering the male hormone is by far the most effective treatment,” he said, but at the same time, however, “there should be more judgment in prescribing GnRH agonists.”
Soloway believes that any increased risk for heart disease and diabetes would be due to a lowering of testosterone. “At this point it makes sense to use hormone therapy when necessary, but not for everyone that has prostate cancer,” he said.
Another expert, Dr. Nelson Neal Stone, a clinical professor of urology and radiation oncology at Mount Sinai School of Medicine in New York City, agreed that, “there is evidence that low testosterone can induce metabolic syndrome.”
For example, he said, there are studies that have shown that men with advanced prostate cancer who take hormone therapy face a twofold increased risk of developing metabolic syndrome, a cluster of symptoms tied to the development of heart disease.
“When I speak to patients who have to go on these agents, I counsel them about the risks of increased weight gain and I tell them they need to monitor their carbohydrate intake and increase their amount of exercise, and they can decrease the risk of developing metabolic syndrome,” he said.
Patients with prostate cancer typically do have some treatment choices. After initial treatment for prostate cancer, whether by surgery or radiation, doctors usually track blood levels of disease-linked prostate-specific antigen (PSA) over time. Based on that, one can initiate hormone therapy, Soloway said, or simply wait and monitor the patient.
“There is further evidence that you should not begin hormone treatment until such time when there is more compelling reason than just a slight rise in PSA,” Soloway said. “There are hundreds and hundreds of thousands of such patients.”
Soloway believes that many men across the United States are unnecessarily taking hormone therapy for prostate tumors that have not yet spread. “I think hormone therapy can be delayed for months to years in some of these men,” he said.
For men with more advanced metastatic prostate cancer, hormone therapy can be used for several months until the PSA goes down, at which point the therapy can be stopped, Soloway said. “If you stop it for the time it takes for the PSA to rise again, that could be many months to a couple or more years,” he said.
Men taking hormone therapy need to understand that, as with any drug treatment, there are some risks, Soloway said. But heart disease is largely preventable, and he believes that GnRH agonists might boost heart risks because they cause men to pile on extra pounds.
So, “you want to do what you can to decrease your chance of diabetes, cardiovascular disease. This has to do with diet, keeping your weight down,” Soloway said.
For Stone, the toughest part is striking a balance between cancer risk and risks from the number one killer of men, heart disease. “It doesn’t make much sense to try and treat their prostate cancer and prevent them from dying from prostate cancer if we are going to increase their risk of them dying from heart disease,” he reasoned.
Once patients understand that, Stone hopes they will be motivated to watch their diet and exercise.
In the meantime, men should not stop taking their hormone therapy, but do everything they can to reduce their risk of developing cardiovascular disease and diabetes with lifestyle changes, he said.
“There is always a price you pay for medications,” Stone said. “But if we’re aware of the consequences of taking the medication, then we can deal with that.”
More information
For more information on prostate cancer, visit the American Cancer Society.