SUNDAY, Dec. 12 (HealthDay News) — Researchers have been able to prod human cells that normally produce sperm to make insulin instead and, after transplanting them, the cells briefly cured mice with type 1 diabetes.
“The goal is to coax these cells into making enough insulin to cure diabetes. These cells don’t secrete enough insulin to cure diabetes in humans yet,” cautioned study senior researcher G. Ian Gallicano, an associate professor in the department of Biochemistry and Molecular and Cellular Biology, and director of the Transgenic Core Facility at Georgetown University Medical Center, in Washington D.C.
Gallicano and his colleagues will be presenting the findings Sunday at the American Society of Cell Biology annual meeting in Philadelphia.
Type 1 diabetes is believed to be an autoimmune disease in which the body mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. As a result, people with type 1 diabetes must rely on insulin injections to be able to process the foods they eat. Without this additional insulin, people with type 1 diabetes could not survive.
Doctors have had some success with pancreas transplants, and with transplants of just the pancreatic beta cells (also known as islet cells). There are several problems with these types of transplants, however. One is that as with any transplant, when the transplanted material comes from a donor, the body sees the new tissue as foreign and attempts to destroy it. So, transplants require immune-suppressing medications. The other concern is that the autoimmune attack that destroyed the original beta cells can destroy the newly transplanted cells.
A benefit of the technique developed by Gallicano and his team is that the cells are coming from the same person they’ll be transplanted in, so the body won’t see the cells as foreign.
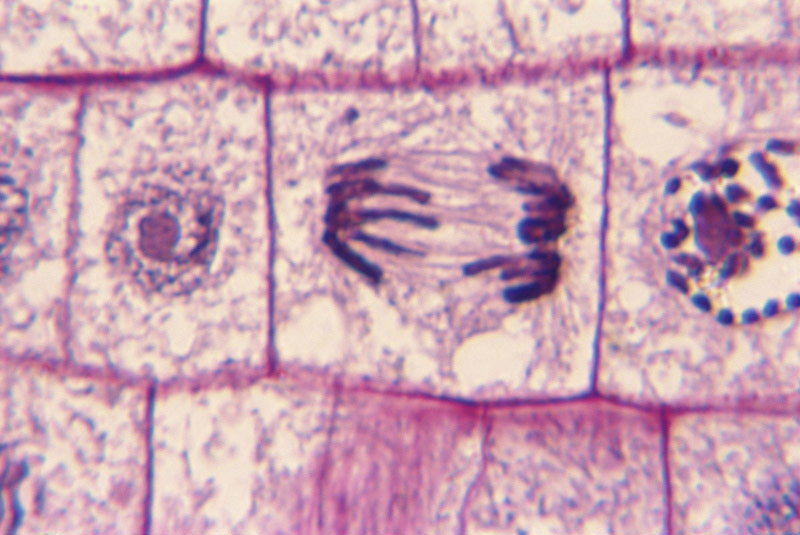
The researchers used spermatogonial cells, extracted from the testicles of deceased human organ donors. In the testes, the function of these cells is to produce sperm, according to Gallicano. However, outside of the testes the cells behave a lot like human eggs do, and there are certain genes that turn them on and make them behave like embryonic-like stem cells, he said.
“Once you take them out of their niche, the genes are primed and ready to go,” he explained.
After removing the spermatogonial cells from the testes, the researchers put them into a special media. According to Gallicano, it’s here that the cells are “chemically” instructed to develop into beta-like cells. In other research attempting to create insulin-producing cells, such as induced pluripotent stem cells, researchers must insert outside genes to get the cells to behave like stem cells. Such outside genes have the potential to lead to additional problems, such as creating cancer.
Once the cells were coaxed into becoming insulin-producing cells, the researchers transplanted them into the mice. The result: blood sugar levels in the mice were reduced for about a week, essentially curing the rodents’ diabetes for a brief time, Gallicano said.
He said he hopes that by transplanting the cells into different areas of the body the researchers may be able to achieve longer blood sugar control.
The only side effect of concern, said Gallicano, is a certain type of tumor called a teratoma. But, he said, it appears with these cells it would take significantly more transplanted cells than would likely be needed before such a tumor might potentially be created.
Funding for the study came from the American Diabetes Association, Georgetown University Medical Center and private donors.
“This study is a positive step, but you still have a risk of teratomas, and the autoimmunity could destroy the new insulin-producing cells,” said one expert, Dr. Camillo Ricordi, scientific director of the Diabetes Research Institute at the University of Miami Miller School of Medicine. “And the other limitation is that this is only for men, not for women.”
But, perhaps a bigger concern in replacing beta cells, said Riccordi, is the potential of causing dangerously low blood sugar levels. Both beta and alpha cells are destroyed in people with type 1 diabetes, and alpha cells produce glucagon, a hormone that increases blood sugar levels in the body when they drop too low. So, if researchers only replace insulin-producing beta cells, and not alpha cells, there is a potential of causing low blood sugar levels, which can also be deadly.
Still, “it is important to explore all avenues in diabetes research,” Riccordi said, “because what you learn in one area may be helpful for others. But don’t place too much hope or hype in one area.”
More information
Learn more about type 1 diabetes from the American Diabetes Association.