TUESDAY, Aug. 10 (HealthDay News) — After studies last year found that a type of surgery called vertebroplasty was no better than a sham procedure in treating painful compression fractures, a new study now suggests the therapy can, in fact, ease some patients’ pain.
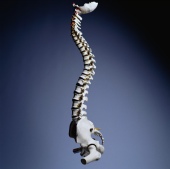
In this (typically) outpatient procedure, doctors inject a type of stabilizing cement into the affected part of the spine.
For some people with weak bones who fracture the small bones in their spine — an injury called an acute osteoporotic vertebral compression fracture — vertebroplasty can be a safe and effective treatment, Dutch researchers conclude in the Aug. 10 online edition of The Lancet.
The study was funded in part by Cook Medical, which makes material used in vertebroplasty.
“Pain relief after the procedure is immediate, sustained for one year, and is significantly better than that achieved with conservative treatment and at acceptable costs,” wrote a team led by Dr. Caroline Klazen, from St. Elisabeth Ziekenhuis in Tilburg, the Netherlands.
But other experts cast doubt on the findings, noting that for most of the study participants, pain resolved on its own without the need for surgery.
The new Dutch study involved 431 patients, aged 50 or older, with osteoporotic vertebral compression fractures. The patients had been in pain for six weeks or less. The researchers randomly assigned them to receive vertebroplasty or conservative treatment.
Conservative treatment included taking pain relievers, ice and heat treatments, and later a stretching and back strengthen program. In addition, a back brace may be called for, experts say.
However, the researchers noted that more than half (53 percent) of participants had their pain spontaneously disappear during the assessment phase of the study.
Among the 202 remaining patients, the 101 treated with vertebroplasty had greater pain relief after a month and a year, compared with those who underwent conservative treatment, Klazen’s group found.
But even among those who did not get vertebroplasty, 60 percent achieved pain relief, leaving only 41 whose pain continued without therapy.
There were no serious side effects or complications from vertebroplasty, the researchers stated.
One important drawback to the study was that patients and doctors knew who received which therapy, Klazen’s team noted. That could have affected patient responses and the radiologists’ assessments, they noted.
Not everyone was convinced by the study findings.
The fact that many people saw their pain clear up on their own, without the surgical intervention, “confirms that we have been managing patients appropriately for all these years — by waiting six weeks [before treatment],” said Dr. David F. Kallmes a professor of radiology at the Mayo Clinic. He was not involved in the study.
Kallmes helped conduct one of the studies published in 2009 in the New England Journal of Medicine that found the surgery was no better than a “sham” procedure in treating compression fracture pain.
Kallmes noted that of the 431 patients selected for the study, more than 50 percent improved without treatment. “And among the 100 who didn’t get treated [with vertebroplasty], 60 percent of those achieved relief at one month. That means that almost 90 percent of the 330 patients who didn’t receive cement achieved a good outcome without cement,” he said.
If those patients who would not improve without treatment could be identified, that “would be great,” Kallmes said. “But we still are unable to” spot those patients, he added, so it’s difficult to predict which patients would gain from the surgical technique.
Compared to standard therapy, cost could become a factor, as well. Although the researchers call vertebroplasty’s price tag “acceptable,” total costs can run about $5,000 including the cost of an MRI scan, Kallmes said.
Another expert, Dr. Eugene J. Carragee, a professor of orthopedic surgery and chief of the spine surgery center at Stanford University, is also not a fan of vertebroplasty for most patients.
“None of the controlled trials, including this one, have even remotely confirmed the 80 to 90 percent rate of complete and immediate pain relief described in original reports of this procedure,” he noted.
In fact, about 60 to 70 percent of the effect seen in the vertebroplasty group was also seen in the control group, Carragee said. “This strongly suggests that most of the improvement in the vertebroplasty group was not due to the procedure alone,” he pointed out.
“The vertebroplasty treatment effect probably includes some direct effect and some placebo effect. But it is unlikely that all of the apparent treatment effect is placebo,” Carragee added.
More information
For more information on compression fractures of the back, visit the U.S. National Library of Medicine.

