WEDNESDAY, July 4 (HealthDay News) — Transplanting just one embryo during assisted reproduction treatments reduces the risk of preventable infant deaths that occur just before or shortly after birth, which is termed perinatal mortality, Australian researchers report.
“The number of embryos transferred per procedure is the major determinant of multiple pregnancy and multiple delivery, which contribute to an elevated risk of preterm birth and low birth weight, and its [health consequences],” said Elizabeth Sullivan, from the perinatal and reproductive epidemiology research unit of the University of New South Wales in Sydney.
“These are risks in addition to those already faced by women being treated for infertility,” Sullivan said in a news release from the European Society of Human Reproduction and Embryology.
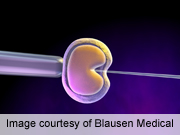
For the study, researchers examined more than 50,200 births resulting from in vitro fertilization (IVF) or intra cytoplasmic sperm injection (ICSI) treatment. IVF involves removing an egg from a woman, placing it with sperm in a test tube, then transferring the resulting embryo to the woman’s womb. With ICSI, a form of IVF, sperm is injected directly into the egg.
The babies were born at more than 20 weeks’ gestation and/or weighed more than 14 ounces (400 grams) at birth. They found 813 perinatal deaths overall, which included 630 stillbirths and 183 deaths within the first 28 days of life.
The researchers calculated the risk of perinatal mortality was 53 percent higher for a two-embryo transfer than for the transfer of one embryo.
They noted this risk was even higher for the transfer of fresh (not frozen) embryos. Births following the transfer of two fresh embryos had a 74 percent higher risk of perinatal death than a fresh single embryo transfer.
The study was scheduled for presentation Wednesday at the annual meeting of the European Society of Human Reproduction and Embryology in Istanbul.
The researchers said the adoption of a single embryo transfer policy for IVF in Australia and New Zealand resulted in a reduction in overall perinatal deaths for all babies conceived by assisted reproduction technology.
“Australia and New Zealand have shown that in the right policy environment, a voluntary change to [single embryo transfer] practice is achievable,” Sullivan noted.
“The proportion of single embryo transfers in Australia/New Zealand IVF rose from 14.2 percent in 1999 to 67.8 percent in 2008,” she said. This was accompanied by a decline in multiple deliveries of 13.7 percentage points — from 22.1 percent in 2000 to 8.4 percent in 2008, Sullivan said.
For non-donor IVF cycles in women younger than 35 years old, the authors recommend single embryo transfer be the rule of thumb.
Data and conclusions presented at meetings should be considered preliminary until published in a peer-reviewed medical journal.
More information
The U.S. National Institutes of Health provides more information on in vitro fertilization (IVF).

