WEDNESDAY, July 13 (HealthDay News) — A mesh device used to support the pelvic organs and help ease incontinence in women appears to carry more risks than previously thought, the U.S. Food and Drug Administration announced Wednesday.
In an “updated safety communication warning,” the FDA said that surgical placement of the mesh through the vagina to fix a condition known as pelvic organ prolapse may lead to greater risks than other surgical methods, while not providing any greater clinical benefit.
“There are clear risks associated with the transvaginal placement of mesh to treat pelvic organ prolapse,” Dr. William Maisel, deputy director and chief scientist of the FDA’s Center for Devices and Radiological Health, said in an agency news release. “The FDA is asking surgeons to carefully consider all other treatment options and to make sure that their patients are fully informed of potential complications from surgical mesh. Mesh is a permanent implant — complete removal may not be possible and may not result in complete resolution of complications.”
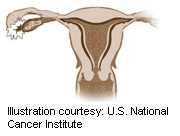
Pelvic organ prolapse involves a weakening or stretching of internal structures that support organs such as the bladder, bowel and uterus. These organs then drop to below their normal position and bulge (prolapse) into the vagina. This can lead to pelvic pain and disruption of sexual, urinary or defecatory function, the FDA explained.
There are numerous means of correcting the problem, such as surgeries carried out through the abdomen or the vagina using traditional stitches, or using the mesh to help improve internal support of the pelvic organs.
However, the FDA says that between 2008 and 2010, the agency received more than 1,500 “adverse event” reports regarding patients who had undergone the mesh procedure — five times as many as were reported between 2005 and 2007. Some of the most commonly cited problems included pain, infection, bleeding, pain during sexual intercourse and urinary problems. Reports were also found of the mesh becoming exposed or protruding from vaginal tissue, or organ perforation from tools used during the surgical placement of the mesh.
More than 100,000 mesh procedures for the treatment of pelvic organ prolapse, 75,000 of which were transvaginal, were carried out in 2010 in the United States, the FDA stated.
The FDA also looked over data from 1996 to 2010 pitting mesh surgeries against non-mesh surgeries and found that the former seemed to carry heightened risks but no greater clinical benefit.
Based on their findings, the agency is urging health-care providers to remember that pelvic organ prolapse can be successfully treated without the use of mesh, with potentially fewer complications or adverse events. The agency urges patients who have had the procedure to check in regularly with their doctors, especially if pain or bleeding develops.
In a statement, the American College of Obstetricians & Gynecologists (ACOG) said it “applauds” the agency move. “The College shares the FDAs concerns and encourages patients and physicians to review the FDA’s White Paper that describes, in detail, the health risks associated with the surgical mesh products when used to treat pelvic organ prolapse,” the ACOG said.
The FDA plans to convene an independent panel of experts to meet and discuss the issue in early September. “Input from the clinicians, manufacturers and other experts will help the FDA better understand the safety and effectiveness of surgical mesh for [pelvic organ prolapse and stress urinary incontinence] repair, including any changes that would improve our oversight,” Maisel said.
More information
Find out more about pelvic organ prolapse at the University of Michigan Health System.

