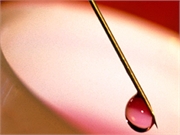
MONDAY, Nov. 4, 2019 (HealthDay News) — There’s early promise in the quest for a blood test that might spot breast cancer up to five years before clinical signs of the disease appear, researchers say.
The test identifies specific immune system “autoantibodies,” British researchers explained. The immune system produces the antibodies when it comes into contact with tumor-associated antigens (TAAs), which are produced by breast tumor cells.
Still, the test is so far only partially effective, so much more research is needed, the investigators said.
The findings were presented Sunday at the U.K. National Cancer Research Institute conference in Glasgow, Scotland.
“The results of our study showed that breast cancer does induce autoantibodies against panels of specific tumor-associated antigens. We were able to detect cancer with reasonable accuracy by identifying these autoantibodies in the blood,” said researcher Daniyah Alfattani, a Ph.D. student at the University of Nottingham’s Centre of Excellence for Autoimmunity in Cancer (CEAC).
“We need to develop and further validate this test,” she added in a conference news release. “However, these results are encouraging and indicate that it’s possible to detect a signal for early breast cancer. Once we have improved the accuracy of the test, then it opens the possibility of using a simple blood test to improve early detection of the disease.”
In the study, Alfattani’s team analyzed blood samples taken from 90 breast cancer patients at the time they were diagnosed. They also analyzed blood samples from 90 women without breast cancer, as a “control” group.
The researchers used a technology called protein microarray to rapidly test the blood samples for autoantibodies against 40 TAAs associated with breast cancer, plus another 27 TAAs that were not known to be linked with the disease.
The accuracy of the blood test was higher with panels that contained more TAAs, the team noted.
For example, a panel of five TAAs correctly detected breast cancer in 29% of the samples from the breast cancer patients, and correctly identified 84% of the samples from the control group as being cancer-free.
A panel of seven TAAs correctly identified cancer in 35% of cancer samples and no cancer in 79% of control samples. A panel of nine antigens correctly identified cancer in 37% of cancer samples and no cancer in 79% of control samples.
One U.S. breast cancer expert was encouraged by the findings, but agreed there’s still a long way to go before blood tests replace mammograms in breast cancer detection.
“It will be great if someday we are able to diagnose breast cancer by a simple test,” said Dr. Lauren Cassell, chief of breast surgery at Lenox Hill Hospital in New York City. “However, the current test, which utilizes nine TAAs, only identified cancer in 37% of known cancer samples. What about the other 63% where it didn’t identify the cancer?” she said.
“This does not appear to achieve the level of accuracy we would like to achieve or which we do reach with our current mammogram and sonogram in terms of detection,” Cassell said.
In the meantime, the British team said they are now testing blood samples from 800 patients against a panel of nine TAAs, and expect the accuracy of the test to improve with these larger numbers.
Alfattani said that “a blood test for early breast cancer detection would be cost-effective, which would be of particular value in low- and middle-income countries. It would also be an easier screening method to implement compared to current methods, such as mammography.”
A similar blood test for lung cancer is currently being tested in a clinical trial in Scotland, and the CEAC group is also working on tests for pancreatic, colorectal and liver cancers.
Dr. Alice Police is regional director of breast cancer surgery at the Northwell Health Cancer Institute in Sleepy Hollow, N.Y. Reading over the new findings, she agreed that “the holy grail of breast cancer detection would be a simple blood test that would tell a patient that they have breast cancer.”
Police said, “We all want an alternative to the mammogram, the ultrasound and the MRI. The problem is that these blood tests don’t tell a patient where the cancer is or what kind or what treatment that they need.”
Because these findings were presented at a medical meeting, they should be considered preliminary until published in a peer-reviewed journal.
More information
The U.S. National Cancer Institute has more on breast cancer.
Copyright © 2025 HealthDay. All rights reserved.