WEDNESDAY, Jan. 13 (HealthDay News) — Belgian transplant surgeons are reporting a medical first: They coaxed a donor trachea to grow its own network of blood vessels before transplantation by first embedding it for months in the recipient’s arm.
The innovative approach not only brought the patient a healthy, functional trachea (windpipe), but it did so without the need for taking lifelong immunosuppressive drugs, as is common with most transplant operations.
“This is very new,” said study author Dr. Pierre Delaere, a professor of otolaryngology at University Hospital Leuven. “People with airway problems can stay alive with tracheal cannula [tubing]. However, a tracheal cannula can give serious breathing and speech difficulties. This new technique may lead to improved quality of life for this group of patients.”
Delaere and his colleagues describe the new procedure in the Jan. 14 issue of the New England Journal of Medicine.
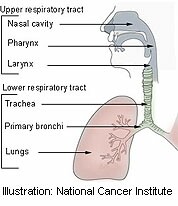
Though many body parts, including kidneys, lungs and other organs, are relatively amenable to transplant, a complex structure like the trachea is not.
“You can’t just transplant the trachea because it doesn’t have a distinct blood vessel supplying it,” explained Dr. Megan Sykes, a transplant immunologist at Harvard Medical School and the author of an accompanying commentary. “You can’t just hook it up to the recipient’s blood vessels.”
But life for people with severely damaged trachea can be very difficult. The patient described in the study was a 55-year-old woman whose windpipe was seriously injured during an emergency tracheotomy after a car accident 25 years earlier. The woman could breathe only with the aid of implanted tracheal stents that caused her to cough continuously and left her vulnerable to a series of infections, including bronchitis and pneumonia.
The Belgian team tried an experimental form of transplant to help the woman. They first found a donor trachea from a deceased man with the same blood type, but the problem of maintaining a blood supply remained.
To get around that problem, the team opened up the woman’s lower left arm and created a kind of pocket for the 3.5-inch-long donor trachea beneath the skin. The trachea “lived” within the woman’s arm forearm for four months. During much of this time, she received standard anti-rejection drugs.
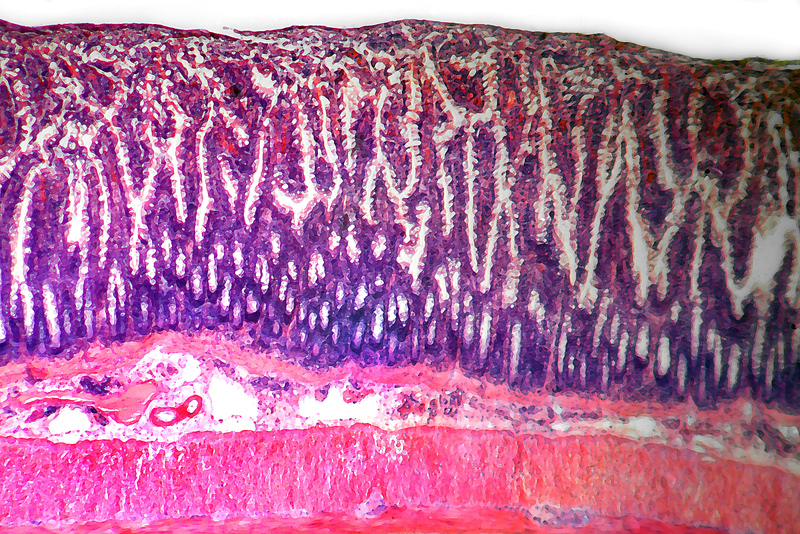
Placing the trachea within the blood- and nutrient-rich environment of the forearm “allowed a process called neovascularization to take place,” wherein the donor windpipe grew a vital network of blood vessels, Sykes explained.
But something else happened, too. The surgeons knew that once anti-rejection drugs were discontinued, the woman’s immune system would attack and destroy the soft mucosal (inner) tissue of the donor trachea. So, a month into the process they opened up the forearm and grafted a piece of soft mucosal lining from the recipient’s mouth onto the donor trachea.
Once immunosuppressive drugs were stopped, the mucosal tissue from the donor was gradually destroyed — as expected — but the transplanted mouth tissue from the patient grew to replace it. In the meantime, the hard cartilage rings of the donor trachea — which give the windpipe its structure — were not rejected, Sykes said, because cartilage is a special kind of tissue that seems to be protected from the immune system.
“So, what was left from the donor — the cartilage in the tracheal rings — is still donor-derived,” said Sykes, who is also associate director of the Transplantation Biology Research Center at Massachusetts General Hospital.
After four months of being embedded in the woman’s forearm, the trachea — now made up of cells from both the recipient and donor — was carefully removed, along with its new blood vessels, and transplanted into her neck.
CT images taken after the operation “showed that the airway had been restored by the tracheal transplant,” the researchers said, and “since the removal of the airway stents, the patient has had no further episodes of bronchitis or pneumonia.”
One year later, the woman remains “satisfied with the outcome” and has no need for anti-rejection drugs, the team said.
According to Delaere, it’s tough to say just how many patients could benefit from this type of procedure in the future. However, because of its high level of safety and the lack of need for immunosuppressive therapy, “this procedure may become the standard of care,” he said.
Sykes noted that transplant specialists have toyed in the past with the notion of boosting the vasculature of transplanted tissue beforehand, “but the idea of doing that in one place [on the body] and then implanting it in another — that’s really new.”
The procedure is “a breakthrough in the context of tracheal reconstruction,” Sykes said. “It’s a way of repairing large tracheal defects that couldn’t be repaired before.”
More information
The United Network for Organ Sharing has more on organ transplant.