THURSDAY, March 17 (HealthDay News) — A recent case in New York City of HIV transmission between a living kidney donor and a transplant recipient highlights the need to revise national policy on the type and timing of HIV tests used to screen living organ donors, say the authors of a new case study.
Routine screening of organ donors for infection with the virus “has made transmission of HIV through organ transplantation rare in the United States,” the researchers noted. “However, despite routine screening, transmission of HIV can be an uncommon complication of organ transplantation and is a public health concern.”
They believe that transplant centers should utilize more sensitive tests to better spot donors who might carry HIV.
The report, published in the March 18 issue of the U.S. Centers for Disease Control and Prevention’s Morbidity and Mortality Weekly Report, describes an investigation launched by the New York City Department of Health and Mental Hygiene in 2010 after it was notified of a potential transplant-related HIV infection. HIV is the virus that causes AIDS.
The case involved an adult kidney failure patient who received a kidney transplant at a city hospital in 2009. The patient did not have HIV before the transplant and, in the year after the transplant, did not engage in any behaviors that would increase the risk of HIV infection. However, HIV infection was confirmed in the patient one year after the transplant.
The kidney donor was an adult male who underwent evaluation as a potential living donor, which revealed a previous diagnosis of syphilis and a history of sex with men. However, laboratory tests conducted during the initial evaluation 79 days before the transplant showed no evidence of HIV infection.
One year after the transplant, the donor underwent screening for sexually transmitted diseases and was found to have HIV. The transplant team was then informed that the donor was HIV-positive.
In an interview during the public health investigation, the donor said he had unprotected sex with one male partner in the year before the donation, including the time between his initial evaluation and the transplant surgery. He did not know the HIV status of his sex partner. The donor also said he had no history of injection drug use, tattoos or blood transfusions.
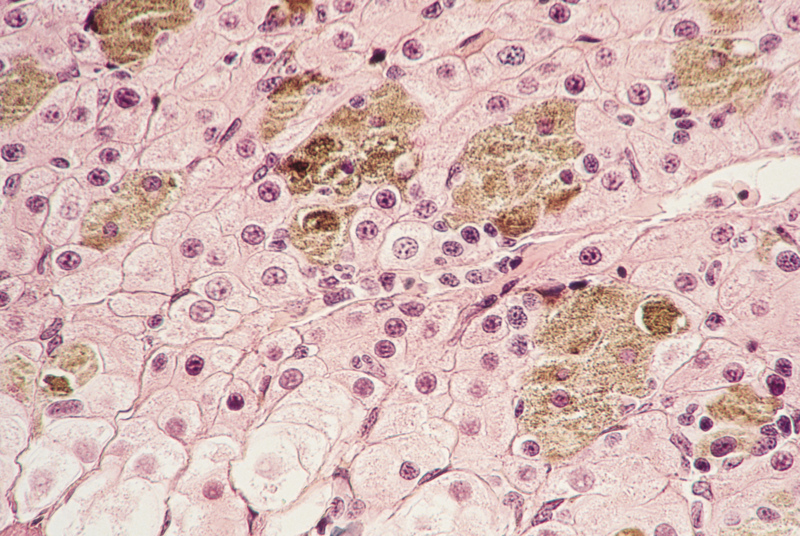
Frozen samples collected from the donor before the transplant were reanalyzed and some of them showed evidence of HIV infection, the study authors noted.
Even though the donor tested negative for HIV prior to the transplant, the most sensitive HIV screening test was not used, as it was not required, according to the report.
“This case highlights the need to revise national policy on the type and timing of HIV tests used to screen living donors,” the case study authors wrote in a CDC news release. “Specifically, transplant centers should screen living donors using the most sensitive test — currently nucleic acid testing (NAT) — as close to the time of transplant surgery as feasible. Donors should also be counseled to avoid behaviors that place them at risk of acquiring HIV because even the most sensitive HIV test can miss recent infections.”
More information
WomensHealth.gov has more about organ transplants.