TUESDAY, Feb. 1 (HealthDay News) — There isn’t sufficient evidence to recommend widespread screening or routine ultrasound tests to check for blocked neck arteries that could cause a stroke.
That’s one key finding from new guidelines on the care of the clogged arteries, released Jan. 31 by the American Heart Association, American Stroke Association and other groups.
A person’s risk of stroke increases when blood flow to the brain is reduced due to clogging of the carotid arteries on the sides of the neck or the vertebral arteries alongside the spine.
While there is no proof that routine screening for blocked neck arteries offers any benefit, “if your doctor hears abnormal blood flow when listening to your neck arteries, or if you have two or more risk factors for stroke (such as high cholesterol or a family history), then [ultrasound testing] is a reasonable approach,” guidelines writing committee co-chair Dr. Jonathan L. Halperin, a professor of medicine at the Mount Sinai School of Medicine in New York, said in an American Heart Association/American College of Cardiology news release.
One expert working in the field agreed with the recommendation.
“The new guidelines suggest that ultrasound should be limited to patients who are at high risk — even if they have not yet had a stroke or mini-stroke,” said Dr. Naveen Goyal, director of the Stroke Center at The Brooklyn Hospital Center, New York City. “It’s not often that patients at risk see a stroke specialist, so these guidelines are primarily directed for all the other physicians who see these patients.”
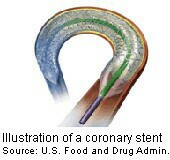
The new guidelines also state that carotid stenting (the placement of an artery-opening mesh tube inside the vessel) and carotid endarterectomy (surgical scraping of plaque from artery wall) are both reasonable and effective ways to open neck arteries that are more than 50 percent blocked.
“The guidelines support carotid surgery [endarterectomy] as a tried-and-true treatment for most patients,” committee co-chair Dr. Thomas G. Brott, a professor of neurology and director of research at the Mayo Clinic campus in Jacksonville. Fla., said in the news release.
“However, for most patients who have a strong preference for less invasive treatments, carotid stenting offers a safe alternative,” he added. “Because of the anatomy of their arteries or other individual considerations, some patients may be more appropriate for surgery and others for stenting.”
One physician agreed that the decision is often made on a case-by-case basis.
“When a high-grade blockage is discovered, these two treatments are now both being acknowledged as acceptable treatment options but the choice between them still remains unclear,” said Dr. Keith A. Siller, medical director of the Comprehensive Stroke Care Center at NYU Langone Medical Center, New York City. That’s because each procedure’s success “is highly dependent on the specialist performing these procedures, the age of the patient, additional anatomical features of the blockage itself, and patient preferences,” he said.
The guidelines also stress that for many patients, medications may remain a better approach than either carotid stenting or carotid endarterectomy.
The guidelines will be published in the journals Stroke and Circulation and in the Journal of the American College of Cardiology.
More information
The U.S. National Institute of Neurological Disorders and Stroke has more about stroke prevention.

