TUESDAY, Aug. 28 (HealthDay News) — People with heart disease who have one blocked artery that restricts blood flow to the heart may do better if they receive a stent to open the artery right away, instead of drug therapy alone, a new study suggests.
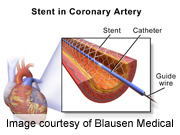
Stents are cylindrical mesh tubes that can be inserted into arteries to prop them open and restore blood flow. In the new study, researchers used a diagnostic tool called fractional flow reserve(FFR) to help determine the best course of treatment among more than 1,200 people with stable heart disease. The test involves placing a special pressurized wire into the artery to measure blood flow to the heart. If blood flow is severely restricted, a stent should be placed immediately.
The study, which was published online Aug. 28 in the New England Journal of Medicine, was stopped early due to high rates of hospitalization and urgent need for stenting seen among people who only received drug therapy (also called “medical therapy”) initially. The study was funded by St. Jude Medical, one of two companies that manufacture the pressure wires used in the new study.
Study author Dr. William Fearon, an associate professor of cardiovascular medicine at the Stanford University School of Medicine, in California, said that the new findings change things for doctors and people with heart disease.
“Patients who have stable coronary disease aren’t all the same. There is a spectrum,” Fearon said. “If we can identify the lesions that are more likely to cause an event, there are benefits to early stent placement compared to medical therapy alone.”
In the study, 888 people had at least one narrowed artery causing restricted blood flow as identified by the FFR test. The rate of heart attack or urgent need for stenting was about 4 percent among those who had a stent placed initially and nearly 13 percent among those who received medical therapy alone at first.
The FFR test is simple to perform and widely available, Fearon said. It costs roughly $700, he noted. “The test saves money in that stents that don’t need to be placed aren’t placed, and it prevents delayed complications associated with urgent need for stent placement,” he said.
“For patients who have symptoms of chest pain who are being referred for testing, it’s reasonable to ask whether or not they have the capability of making the FFR measurements as it will help guide decisions and improve patient outcomes,” Fearon said.
Commenting on the report, Dr. Manesh Patel, a cardiologist at Duke University Medical Center in Durham, N.C., said: “It’s not just whether or not you have stenosis or blockage, but whether or not it is causing restricted blood flow to the heart.”
Patel explained that “using this strategy to decide who should receive a stent reduces risk of coming back urgently and needing a stent.” Any person with blocked arteries should also be taking medication that usually includes aspirin and cholesterol-lowering statin drugs. “We should be treating with medication and if the FFR test reveals that the blockage is reducing blood flow, we should stent,” he said.
Not everyone is convinced that this is the way to go. In an accompanying journal editorial, Dr. William Boden, a cardiologist at Albany Medical College in Albany, N.Y., pointed out that the new study only tells us about the short-term risk of unplanned emergency stenting, but does not provide any evidence on long-term benefits or risks. Ongoing studies, including one in which Boden is an investigator, will provide such answers, he noted.
More information
The U.S. National Library of Medicine has more about stents.

