FRIDAY, Oct. 3, 2014 (HealthDay News) — When given to pregnant women, a common treatment for ulcerative colitis may inadvertently lower their baby’s ability to fight off infections at birth, new French research suggests.
The treatment, called anti-TNF therapy, is an injected, artificial antibody. This type of medication is widely seen as a safe and effective way to tackle a wide range of autoimmune disorders, such as rheumatoid arthritis and inflammatory bowel conditions that include ulcerative colitis and Crohn’s disease. It’s not unusual for pregnant women to receive the treatment, given that inflammatory bowel diseases often strike women of childbearing age.
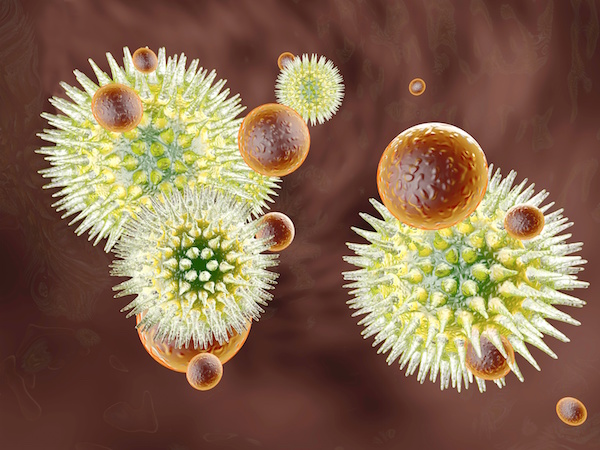
However, this type of drug can cross the placenta and reach the fetus, the study authors said. And four French cases — all involving babies born to women exposed to Remicade (infliximab) during pregnancy — suggest the therapy may cause newborn neutropenia, which is an abnormally low white blood cell count.
The result: severe skin lesions and blistering due to the baby’s inability to produce enough neutrophils, a key type of white blood cell needed to fight off bacterial and fungal infections.
But two U.S. experts questioned the study findings. They said the drugs are considered safe and effective — and potential harms if the drugs aren’t taken during pregnancy can include miscarriage or premature delivery.
Dr. Loic de Pontual, of the Service de Pediatrie at the Hopital Jean Verdier in Bondy, France, and colleagues reported their findings in the October issue of the journal Pediatrics.
According to the Crohn’s & Colitis Foundation of America, ulcerative colitis may affect as many as 700,000 Americans. It develops when a person’s immune system goes out of whack, erroneously interpreting the normal digestive process (such as incoming food) as an attack on the large intestine.
For many patients, this leads to significant abdominal discomfort and cramping alongside persistent diarrhea, all stemming from severe inflammation of the intestinal lining. For many, anti-TNF treatment is the answer.
“TNF is a chemical of inflammation that is overproduced in ulcerative colitis and a number of other inflammatory disorders,” said Dr. Stephen Hanauer, director of the digestive health center at Northwestern University’s Feinberg School of Medicine, in Chicago. “So, infliximab is an anti-TNF drug that neutralizes it. And I would say it’s highly effective and, in general, very safe.”
Dr. Jonathan Ramprasad, a pediatric gastroenterologist with McLane Children’s Scott & White Hospital in Temple, Texas, agreed.
“The treatment is common, safe and state-of-the-art,” he said. “It’s a very specific biologic intervention that is widely used for many conditions.”
Neither doctor participated in the French study cases, all four of which involved the onset of either moderate or severe neutropenia within the first few days or weeks of life.
In the first case, the mother-to-be (aged 24) had been receiving infliximab every seven weeks for two years before becoming pregnant. Once pregnant, her treatment was reduced to once every eight weeks, and then halted altogether at roughly the 27th week of the pregnancy.
The other three cases involved a 28-year-old woman who was pregnant with triplets, and who had also been treated with infliximab until the 27th week of pregnancy.
Antibiotics prompted a full recovery among all four babies within eight to 14 weeks, the study authors reported.
Because neutrophil counts are not normally monitored among children born to mothers receiving anti-TNF treatments, the French researchers suggested that their findings argue in favor of conducting routine white blood cell testing in all such cases, both at birth and throughout the first few weeks of life.
But Hanauer said that the findings “are no reason to be alarmed.”
“Yes, these drugs do cross the placenta and get into the baby,” he explained. “There’s no question about that. But prior studies to date have not demonstrated any increased risk to babies. And this report does not indicate what other medications these mothers were on while pregnant. It’s just not mentioned. So we don’t know,” Hanauer said.
“So, I’d say that the [U.S.] Food and Drug Administration has classified infliximab as a ‘Class B’ medication, which means it’s presumed to be safe. And in the U.S. we have not yet seen any significant cause to change that designation. And the key point is that the best outcome for a baby is a healthy mother during pregnancy,” Hanauer added.
“I’m not discounting these findings. But there have been no cases like this reported in the U.S., so they will need to reconfirmed,” Hanauer said. “Until then, there is no reason to believe this treatment is not safe for both mother and child.”
The association seen in the study does not prove a cause-and-effect relationship.
In their report, the French researchers also noted that the cases they found are the first, and that further research is required. And they add this caveat to their finding:
“In the vast majority of cases, the benefits of anti TNF[-alpha] agents outweigh the risks during pregnancy,” de Pontual and colleagues wrote. “Indeed, active inflammatory bowel disease in the mother can lead to adverse pregnancy outcomes, such as [miscarriage] or preterm delivery.”
More information
Visit the Crohn’s & Colitis Foundation of America for more on ulcerative colitis.
Copyright © 2026 HealthDay. All rights reserved.