WEDNESDAY, May 16 (HealthDay News) — A drug approved to treat advanced prostate cancer appears to help men who have localized high-risk prostate cancer if given before surgery.
Adding Zytiga (abiraterone) to conventional hormonal treatments eliminated or nearly eliminated the prostate cancer in one-third of men with this often-lethal form, according to new research to be presented at next month’s annual meeting of the American Society of Clinical Oncology (ASCO) in Chicago.
“This is one of the first — if not the first — study to show that you can make prostate cancer in the prostate gland itself disappear in a reproducible number of patients,” ASCO official Dr. Nicholas Vogelzang said at a Wednesday press conference.
Commenting on the findings, Dr. Jay Brooks, chairman of hematology/oncology at Ochsner Health System in Baton Rouge, said, “This is exciting. It’s a novel way to eliminate cancer before surgery.”
However, Brooks, who was not involved in the study, cautioned that the findings were still preliminary and need further investigation.
Trying to shrink a tumor with chemotherapy and/or radiation before surgery is standard for other types of cancer, such as breast or colon, but hasn’t to date shown a benefit in prostate cancer, study author Dr. Mary-Ellen Taplin, associate professor of medicine at Harvard Medical School and Dana-Farber Cancer Institute in Boston, explained at the news conference.
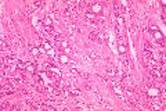
Localized high-risk prostate cancer, which is defined as prostate cancer in men with a prostate-specific antigen level above 20, high-grade disease (a Gleason score of 8 or more), and stage T3 disease (indicating the tumor has spread through the prostate), carries with it a poor prognosis.
Standard hormonal therapy, which stops the production of male hormones (androgens), has not been shown to be effective in this type of cancer when given before surgery. Nor has the surgery, which removes the entire prostate.
Zytiga blocks production of testosterone, which can promote the growth of prostate cancer cells, but in a different way than established hormonal treatments.
This small, phase 2 trial involved 56 men with an average age of 58, all of whom had had at least three positive biopsies for prostate cancer.
For the first three months, 27 men received the standard hormonal therapy leuprolide alone, followed by leuprolide plus Zytiga for another three months.
The remaining 29 men received the two-drug combination for the whole six months, after which all men in both groups underwent prostate surgery.
One-third of the men who had received leuprolide plus Zytiga for the entire six months saw complete or nearly complete elimination of their cancer.
By comparison, only 15 percent of men in the other group experienced these results, the investigators found.
Those who received the combination for only 12 weeks had much lower response rates.
The participants also received low doses of the steroid prednisone to prevent side effects from Zytiga, although side effects overall were minimal, said Taplin.
It’s not clear at this point why some men responded to the combination therapy while others did not, and that is an area that needs to be studied, the researchers said.
“In highly select people who have this aggressive type of prostate cancer, I think this is an important area to investigate,” Brooks noted. “We need to figure out which patients would potentially benefit.”
According to study author Taplin, the research received some funding from
Johnson & Johnson, the maker of Zytiga. She said the drug is currently
U.S. Food and Drug Administration-approved for patients with advanced prostate cancer that does not respond to hormone therapy, and costs about $5,000 per month.
The data and conclusions of research presented at medical meetings should be viewed as preliminary until published in a peer-reviewed journal.
More information
The U.S. National Cancer Institute has more on treatments for prostate cancer.

