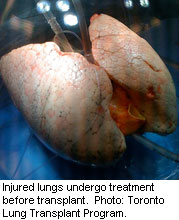
WEDNESDAY, April 13 (HealthDay News) — Using a technique that looks like it could have been pulled from a science fiction thriller, transplant surgeons can now keep lungs alive outside of the body, giving them time to heal and allowing surgeons to better assess the health of the lungs before transplant.
In the new procedure, lungs are placed in a protective glass dome after being removed from the donor. They’re then hooked up to a ventilator, so the lungs can continue to breathe, and the lungs are given what’s known as a perfusion solution to mimic blood circulating through them.
“We’ve developed a technique that allows us to assess and treat lungs outside of the body,” said the study’s senior author, Dr. Shaf Keshavjee, director of the Toronto Lung Transplant Program at Toronto General Hospital.
“The pleasant surprise from our study was that we set out to prove these lungs would be equivalent, but we now have data showing that these patients can even do better,” he said.
Results of the study are published in the April 14 issue of the New England Journal of Medicine.
Currently, more than 80 percent of donor lungs are unsuitable for transplant, with fewer than 15 percent of lungs from multiorgan donors able to be used, according to the study. Because of the relatively small number of organs that are deemed to be acceptable, mortality is high among patients awaiting transplantation, the authors pointed out.
Keshavjee said that the reason so few lungs are suitable for transplant is that brain death and complications from treatments received often damage the lungs. Then, when the lungs are removed from the body, they don’t have a chance to begin healing.
“What we’ve tried to do is make the lungs think they’re still in the body. This allows them the chance to recover,” said Keshavjee.
Lungs are only placed on the machine for two to four hours, but that’s enough time for them to start to heal, he said. The other big benefit is that because the lungs are essentially alive in the glass dome, surgeons can assess the health and function of the lungs before transplant.
Keshavjee said he thinks this procedure could triple, or even quadruple the number of available donor lungs.
In the current study, 136 lungs were transplanted. Twenty-three of those lungs were selected to undergo the new technique, which is known technically as normothermic ex vivo lung perfusion. These lungs were chosen because they would normally have been considered high risk for normal transplant. In addition to ventilation and circulation, the lungs also received antibiotic and anti-inflammatory medications.
After four hours, 20 of the lungs undergoing the new procedure were deemed suitable for transplant. The other three sets weren’t functioning well enough to be transplanted.
Compared to 30 percent of the lungs selected in the conventional way, only 15 percent of the ex vivo-treated lungs had what’s known as primary graft dysfunction. This is a serious complication of transplant, and means that the lungs aren’t getting circulation as they should. Primary graft dysfunction, in fact, can lead to rejection of the transplanted organ.
The study was sponsored by Vitrolife, a biotechnology company that supplied materials and equipment for the research but otherwise had no control over the study.
There was no increased risk of adverse events in the treatment group, according to the study. Two of 20 patients died within 30 days of transplantation in the ex vivo perfusion group — although the cause of the deaths was not directly related to the transplant — as compared with six of 116 in the control group, the researchers noted.
After a year, the survival rate was 80 percent for the patients with ex vivo-treated lungs and 83.6 percent for the control group, according to the report.
In addition to increasing the available number of lungs for transplant, Keshavjee said that this new technique will also eventually allow doctors to treat disease in potential donor lungs before transplanting them. “We’re entering an era of personalized medicine and with molecular and gene-based therapies, we may be able to fix organs before using them,” he said.
In addition to lungs, Keshavjee said that this technique could likely be used for other organs to increase the number of available organs for transplant. He said liver surgeons at Toronto General Hospital have started working on adapting this technique for donated livers.
“This study is extremely exciting. It’s really on the frontier of what we’re able to do in terms of organ preservation and transplantation,” said Dr. Michael Goldstein, director of kidney and pancreas transplantation at Mount Sinai Medical Center and medical director of the New York Organ Donor Network in New York City.
Goldstein also pointed out that this technique could allow donated lungs to become more widely available geographically. He said that, currently, donated lungs typically can’t travel very far, which means that the person who might be most in need might not get the donated lungs simply because of distance. But, if the lungs remain viable for longer periods of time, that geographical limitation might be eliminated.
Dr. Joseph Pilewski, medical director of the lung transplantation program at the University of Pittsburgh Medical Center, said that having the extra time this technique provides might also allow surgeons to better match donated lungs to potential recipients, possibly reducing the risk of rejection.
Neither Goldstein nor Pilewski expressed any concerns about the medical aspects of the new lung-preserving procedure. Both pointed out that the device and technique are labor intensive, and currently require a significant infrastructure investment, but both expect that the technique will be refined to become more accessible.
“This group in Toronto has really made significant progress in a short period of time. Right now, this may end up being limited to a few centers, but other companies will probably jump in. In the long run, about three to five years, I think this technique has great potential to change the way we practice. This technique is promising and has a large number of potential uses,” said Pilewski.
More information
Learn more about lung transplants from the U.S. National Heart, Lung and Blood Institute.

