WEDNESDAY, Jan. 29, 2014 (HealthDay News) — People who need skin grafts because of burns or other injuries might someday get lab-grown, bioengineered skin that works much like real human skin, Swiss researchers report.
This new skin not only has its own blood vessels but also — and just as important — its own lymphatic vessels. The lymph vessels are needed to prevent the accumulation of fluids that can kill the graft before it has time to become part of the patient’s own skin, the researchers said.
The discovery that lymph vessels can be grown in a laboratory also opens up “a broad spectrum of possibilities in the field of tissue engineering, since all organs in the human body — with the exception of the brain and inner ear — contain lymph vessels,” said lead researcher Daniela Marino, from the Tissue Biology Research Unit at University Children’s Hospital Zurich.
“These data strongly suggest that if an engineered skin graft containing both blood and lymph vessels would be transplanted on human patients, fluid formation would be hindered, wound healing would be improved and regeneration of a near natural skin would be greatly promoted,” Marino said.
The researchers said that until now, bioengineered skin grafts had not contained much of the components of real skin, including blood and lymphatic vessels, pigmentation, sweat glands, nerves and hair follicles.
Blood vessels transport nutrients, oxygen and other essential factors that keep organs alive and functioning. Lymph vessels remove fluid from the tissue and return it to the bloodstream.
“When skin is wounded, fluid builds up in the damaged tissue,” Marino said. “If not efficiently removed, it accumulates to form so-called seromas, which may impair wound closure and skin regeneration.”
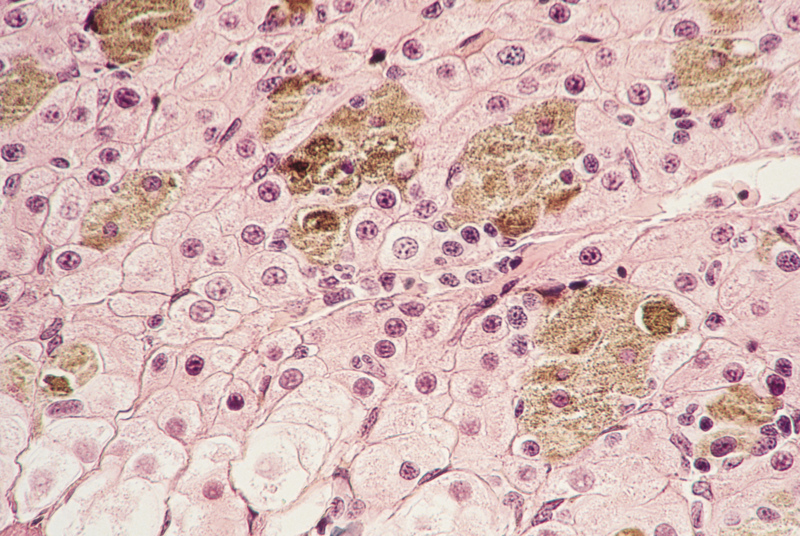
To create the new skin, Marino’s group used human cells from blood and lymph vessels, placing them in a solution that scattered the cells onto a skin-like gel. After time in an incubator, the mixture grew into skin grafts.
The researchers then tested the grafts on rats, and found that the bioengineered skin turned into near-normal skin. After connecting the graft to the rats’ own lymph system, it collected and drew fluid away from the tissue — just as normal skin does.
Skin grafts grown this way might find their best use in patients with severe burns who do not have enough of their own healthy skin available for grafts, the researchers said.
Experts note, however, that experiments in animals don’t always work out when tested in people. But Marino said she is hopeful that trials in humans are not too far away.
Not everyone is sure there will be a big role for these types of grafts, however.
Dr. Alfred Culliford, director of plastic, reconstructive and hand surgery at Staten Island University Hospital in New York City, called the bioengineered tissue “a technology in search of a purpose.”
“I don’t think it will be broadly applicable to many people who need skin grafts,” Culliford said. “It may be helpful in burn patients who have had a large portion of their body surface burned and don’t have enough healthy skin to transplant.”
Culliford said the best grafts for most patients still come from the patient’s own skin. In addition, he said he doesn’t believe adding lymph vessels to a graft is a great advance, since fluid drainage is now done by methods such as compressing the graft.
But Dr. Robert Glatter, an emergency physician and burn expert at Lenox Hill Hospital in New York City, saw more promise in the technology.
“Although we are still in animal models, in the near term there is a significant possibility this could remarkably change the way we deal with non-healing wounds,” Glatter said.
Non-healing wounds are generally found among people with diabetes or vascular disease whose own skin doesn’t function normally. “They don’t heal well with standard skin grafts,” Glatter said.
For her part, Marino said the newer tissue is a real advance.
“Taken together, it is most important to have both blood and lymph vessels in a bioengineered skin to initiate nutrition soon after transplantation and to maintain the balance of tissue fluids,” she said. “This long-awaited step in regenerative medicine is now in reach.”
The report was published Jan. 29 in the journal Science Translational Medicine.
More information
For more information on skin grafts, visit the U.S. National Library of Medicine.
Copyright © 2026 HealthDay. All rights reserved.