WEDNESDAY, Dec. 16 (HealthDay News) — E. coli bacteria in food — commonly linked to food poisoning and the stomach pain and diarrhea that result — might also be the cause of some urinary tract infections.
Researchers have found the same strains of the bacteria in chicken from stores and restaurants and in women with the infections.
There’s no evidence that the germs were transmitted directly to the women through the food they ate, although that’s possible. Still, the findings are the first to suggest a possible link between the food supply and urinary tract infections, said Amee R. Manges, an assistant professor at McGill University in Montreal and lead author of a report on the discovery. It is published in the January issue of Emerging Infectious Diseases.
“This may be happening more frequently then we expected,” Manges said. In addition, she said, the transmission through food could boost the number of urinary tract infections that are resistant to drugs.
Though most strains are harmless, dangerous strains of E. coli germs can be transmitted through food that was contaminated in the field or was not properly handled or cooked, causing problems in the intestinal system. It’s less known that the germs can also spread to the urinary tract in women and men.
In women, that can happen during sex, Manges said. “It’s possible for bacteria to travel from the anus to the vagina and urethra, and that’s where it ultimately causes the infection,” she said.
Urinary tract infections caused by transmission from feces “are most common in older and debilitated individuals in whom the risk of fecal contamination of the urethral orifice is a significant risk, especially in a setting of fecal incontinence,” added Dr. Pascal James Imperato, dean of the School of Public Health at the State University of New York Downstate Medical Center in Brooklyn, N.Y.
It’s also possible for the germs to be transmitted through use of the restroom after handling of contaminated food, said Marion Nestle, a professor in the nutrition, food studies and public health department at New York University.
In their study, Manges and her research colleagues wanted to find out if the same strains of E. coli were present in both meat and in women with urinary tract infections.
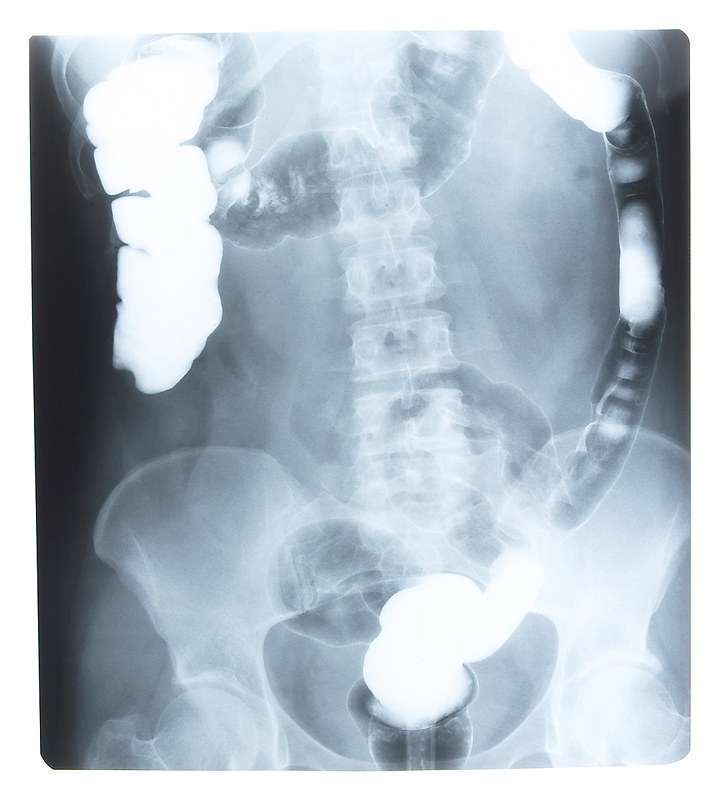
They studied 353 samples from Canadian women, ages 18 to 45, who had suspected urinary tract infections. They also examined samples of chicken and honeydew melon from stores and restaurants in Canada.
The researchers found that several strains of E. coli found in the women and in the food were indistinguishable or closely related.
But there’s a big caveat. “We haven’t demonstrated that this woman ate this piece of chicken meat, and therefore her infection was caused by that piece of chicken,” Manges said.
That’s a problem, Imperato said. “Unless one has positive evidence, gathered through a thorough history, that someone ate an E. coli-contaminated food, one cannot definitively conclude that any of these foods were the source of their illness.”
What to do? As usual, “consumers should be careful to follow standard food-safety procedures when preparing meat or eating undercooked food, including frequent hand-washing,” Nestle advised.
More information
The U.S. National Institute of Allergy and Infectious Diseases has more on E. coli.