TUESDAY, Aug. 7 (HealthDay News) — Despite their increasing popularity as a treatment for sinusitis, corticosteroids do not seem to ease the symptoms of this common infection, a new Dutch study suggests.
“This condition can considerably impair daily functioning, and its unpleasant symptoms may have a negative influence on the quality of life,” said study author Dr. Roderick Venekamp, a postdoctoral researcher and general practitioner trainee in the department of otorhinolaryngology at the University Medical Centre Utrecht.
“As a consequence, patients’ needs toward an effective therapy are often high. This might explain the high antibiotic prescribing rates in daily practice,” Venekamp said. “However, previous studies revealed that the vast majority of patients with mild to moderate acute rhinosinusitis do not benefit from antibiotics.”
“Nowadays, intranasal corticosteroids — anti-inflammatory drugs — are increasingly being used to alleviate symptoms,” he said. “Evidence regarding their benefits is, however, inconclusive, [and] based on our findings we conclude there is no rationale for using corticosteroids in patients with symptoms consistent with acute rhinosinusitis.”
The study appears in the current issue of the Canadian Medical Association Journal.
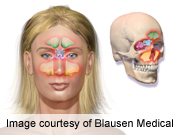
The authors note that acute sinusitis — which strikes about 31 million Americans every year — is principally viral in origin, a byproduct of the common cold. That said, allergies and bacterial infection also sometimes play a role.
Nasal inflammation and blockage are key symptoms of the condition, as are headaches accompanied by facial pain and pressure.
Previous research, including an Oxford University review of six prior investigations involving corticosteroid nasal sprays that was published in the May/June issue of the Annals of Family Medicine, have shown this approach to be of questionable benefit. It is also expensive, costing about $60 per bottle.
To further explore the issue, the Dutch team focused on nearly 200 adult patients receiving care for acute rhinosinusitis at one of 54 primary care practices in a southwestern region of the Netherlands.
Roughly half the patients were randomly selected to receive a week-long regimen of 30 milligrams of the corticosteroid prednisolone each day, while the other half received a dummy treatment that contained no corticosteroids.
All the patients were asked to keep a symptom diary to track the status of their condition for the ensuing two weeks.
The result: By the end of the week, very little difference was seen in the way each group fared.
For example, nearly 63 percent of those treated with a corticosteroid experienced full relief of their prior facial pain or pressure, compared with nearly 56 percent among those given a placebo — a difference that was not deemed clinically significant.
What’s more, there was no appreciable difference observed between the two groups in terms of either quality-of-life measurements or the dissipation of all symptoms (including nasal, cough and congestion issues, as well as pain and discomfort).
“We strongly recommend physicians refrain from treatment with antibiotics and corticosteroids, and advocate symptomatic treatment [acetaminophen and xylometazoline nose drops] in patients with mild to moderate acute rhino sinusitis,” the study authors said.
However, Dr. Michael Stewart, chairman of the department of otolaryngology at New York Presbyterian-Weill Cornell Medical Center in New York City, countered that often the problem is not due to corticosteroid therapy itself but rather to a poor understanding of which patients are good candidates for the treatment.
“I believe that it’s likely that in a true case of bacterial sinusitis a short course of steroids will help the patient get better quicker,” he said. “You won’t improve the overall cure rate or where the patient will be after the infection is over, but you may make them better in the short term.”
“But the problem,” Stewart explained, “is that probably only 10 percent of people who go to a primary care physician thinking they have a bacterial sinus infection actually do, because it shares so many symptoms with a viral upper respiratory infection, such as congestion pressure, coughing and discolored drainage.”
“That means about 90 percent actually have a viral infection,” he added. “Even among patients already referred to a specialist, only about 40 percent or 50 percent actually have a bacterial infection, which means half or so have a virus, for which oral decongestants and Tylenol are the answer, not corticosteroids.”
“I think this study is putting out a good general message that both antibiotics and steroids are subject to overuse,” Stewart acknowledged. “But I would say that for the subset of patients who have a true bacterial sinusitis infection, steroid treatments may actually make an impact.”
More information
For more on sinusitis, visit the U.S. National Institutes of Health.