TUESDAY, April 2 (HealthDay News) — Adults with recurrent sore throats might benefit from getting their tonsils removed, according to a new study from Finland.
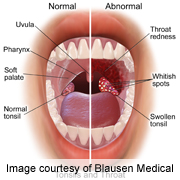
People tend to think of tonsillitis — sore and swollen tissues at the back of the throat — as occurring in childhood. However, many adults suffer from recurrent sore throats that result when tonsils are inflamed by bacteria living within.
These constant infections can lead to repeated courses of antibiotics and reduce a patient’s quality of life, experts say.
“Adult patients who had disabling pharyngitis [severe sore throat] involving the palatine tonsils more than three times per year benefited from tonsillectomy,” said lead study author Dr. Timo Koskenkorva, of the department of otorhinolaryngology at the Institute of Clinical Medicine at the University of Oulu.
“The rate of inflammation of the throat and number of symptomatic days were significantly lower in the tonsillectomy group than in the control group [study participants who did not have their tonsils removed], resulting in fewer medical visits and absences from school or work,” he said.
However, inflammation and sore throats prevented by surgery would likely have been mild and caused by a virus rather than bacteria, Koskenkorva noted. And the surgery does carry some risk and a need for recovery time.
Dr. Linda Dahl, an ear, nose and throat specialist at Lenox Hill Hospital in New York City, said that adults who might consider a tonsillectomy are those who frequently get sick with sore throats. “No one ever regrets having their tonsils out,” she said. “It has an impact on lifestyle.”
In addition to not getting the infections, their body isn’t fighting the bacteria living in the tonsils, which can make them feel rundown, said Dahl, who was not involved in the new study.
The report was published April 2 in the CMAJ (Canadian Medical Association Journal).
To test the benefits of having a tonsillectomy, Koskenkorva’s team randomly assigned 86 patients to have the operation or not.
After five months, none of the patients who had a tonsillectomy had a severe sore throat, compared with 3 percent of those who didn’t have the operation, the researchers found.
Of those who had a tonsillectomy, 4 percent saw a doctor for a sore throat compared with 43 percent who didn’t have the procedure. In addition, 80 percent of patients who didn’t have their tonsils out had an acute sore throat compared with 39 percent who had had tonsillectomies, the researchers noted.
“Tonsillectomy resulted in fewer symptoms of pharyngitis, consequently decreasing the number of medical visits and days absent from school or work. For this reason, surgery may benefit some patients,” Koskenkorva said.
During the six-month follow-up period, people who had tonsillectomy had a lower overall rate of sore throats and significantly fewer days with throat pain, fever, cold or cough than participants who didn’t undergo the procedure, the study found.
However, the surgery prevented mostly mild sore throats, which were most likely caused by a virus, Koskenkorva said. So before having the surgery, which is done under general anesthesia, patients and their doctors should consider complications and whether the benefits outweigh the risk of the operation, he suggested.
One risk of tonsillectomy is bleeding. Dahl, the New York specialist, said that adults, because their tonsils tend to be very infected, can bleed more. “It’s just a little bit of a bloodier surgery,” she explained.
“There are less painful and less risky ways of doing the surgery now,” she added. These include shaving away the tonsils and laser procedures.
The recovery from traditional surgery can cause pain and difficulty swallowing for up to 10 days. Dahl said one patient told her “it’s worse than childbirth without anesthesia.” Recovery from other methods is shorter and less painful, she noted.
More information
To learn more about tonsillectomy, visit the U.S. National Library of Medicine.

