WEDNESDAY, March 19, 2014 (HealthDay News) — Removing half the skull is a drastic step, but it’s one that can save lives in people over 60 who’ve had a severe stroke, new research indicates.
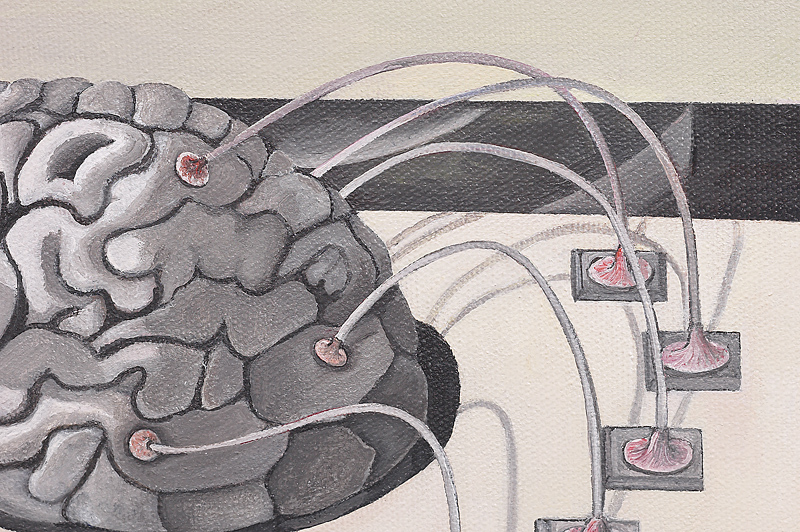
Unfortunately, even though the procedure — called hemicraniectomy — reduces pressure on a swelling brain, the surgery doesn’t prevent disability caused by the stroke.
“Hemicraniectomy in malignant middle cerebral artery stroke, which is proven lifesaving and prevents severe disabilities in patients under 60, remains lifesaving in elderly patients with malignant [stroke]. Seventy percent survive with surgery, only 30 percent without,” said senior study author Dr. Werner Hacke.
“Some of these older stroke survivors do have a severe disability, which may require help in most daily activities,” added Hacke, a professor of neurology and chairman of the neurological center at the University of Heidelberg, in Germany.
Results of the study are published in the March 20 issue of the New England Journal of Medicine.
There are two types of stroke: hemorrhagic and ischemic stroke, the second of which is far more common. Ischemic stroke, which occurs when a blood vessel in the brain is blocked, is the type researchers looked at in this study.
During a large ischemic stroke, one possible complication is brain swelling. When swelling is severe, the brain starts to compress as it reaches the skull. This occurs in about 5 percent of strokes, according to the author of an accompanying editorial, Dr. Allan Ropper, executive vice chair of neurology at Brigham and Women’s Hospital, in Boston.
One way of relieving that pressure is to remove (and eventually replace) a portion of the skull above the affected brain tissue. This procedure is called hemicraniectomy. Previous research has focused on hemicraniectomy in people under 60 who’ve had a stroke. In younger people, hemicraniectomy — when done within the first 48 hours after a stroke — leads to better survival rates and less severe disability.
But, because most strokes occur in those over 60, the researchers wanted to know if hemicraniectomy offered the same benefits to older people.
The current study included 112 people aged 61 and older, with an average age of 70. They all had ischemic strokes affecting the middle cerebral artery. They were randomly assigned to receive either conservative treatment in the intensive care unit or hemicraniectomy within 48 hours of the start of symptoms.
The odds of survival were more than twice as high for those in the surgery group compared to the conservatively treated group, according to the study.
None of the patients in either group survived with no disability or a slight disability. Seven percent of those in the surgery group and 3 percent in the conservative treatment group had a moderate disability, while 32 percent of the surgical group had a moderately severe disability compared to 15 percent in the nonsurgical group.
Twenty-eight percent of those who had hemicraniectomy had a severe disability versus 13 percent of the conservative treatment group.
Most of those who survived their strokes needed help with most bodily needs, such as walking, dressing and eating, according to the study.
Hacke said walking was unlikely for most of these people, and the ability to talk depended on which side of the brain the stroke occurred. He said it took about eight to 12 weeks before the skull or a skull prosthesis could be placed over the brain.
“The value of this study is that it gives more hard numbers by which to gauge what are the likely outcomes,” editorial author Ropper said. “There does not appear to be a beneficial or a detrimental effect on the stroke deficit from surgery. But, hemicraniectomy is lifesaving, and that’s been validated in this study. So, for an individual or a family who would’ve viewed survival after stroke as a satisfactory outcome, surgery is a reasonable thing to do,” he added.
Study author Hacke noted, “You may survive a usually deadly stroke, but the quality of life is not always good afterwards. Patients and relatives must be involved [in the decision-making], and it helps to know what the patient’s preference would be.”
Ropper said that sometimes patients who’ve had a stroke can be involved in the choice, but that it’s often left up to the family to make a quick decision.
Surprisingly, the risks associated specifically with the surgery aren’t significant. They include a risk of bleeding and infection, according to Hacke, who added that the complications from this surgery are generally easy to control.
Hacke said his center sees about 30 patients a year who are candidates for hemicraniectomy. Ropper said the procedure is also done in the United States.
More information
Learn more about stroke from the U.S. National Library of Medicine.
Copyright © 2025 HealthDay. All rights reserved.