MONDAY, Jan. 11, 2016 (HealthDay News) — A type of heartburn medication called proton pump inhibitors may be linked to long-term kidney damage, a new study suggests.
Prilosec, Nexium and Prevacid belong to this class of drugs, which treat heartburn and acid reflux by lowering the amount of acid produced by the stomach.
People who use proton pump inhibitors (PPIs) have a 20 percent to 50 percent higher risk of chronic kidney disease compared with nonusers, said lead author Dr. Morgan Grams, an assistant professor of epidemiology at Johns Hopkins University in Baltimore.
The study was published Jan. 11 in JAMA Internal Medicine.
The study doesn’t establish a direct cause-and-effect relationship between the drugs and chronic kidney disease. However, Grams said, “We found there was an increasing risk associated with an increasing dose. That suggests that perhaps this observed effect is real.”
Proton pump inhibitors were used by more than 15 million Americans in 2013, according to background notes.
But as many as 70 percent of these prescriptions have been handed out inappropriately, and 25 percent of long-term users could stop taking the medication without suffering increased heartburn or acid reflux, the study authors said.
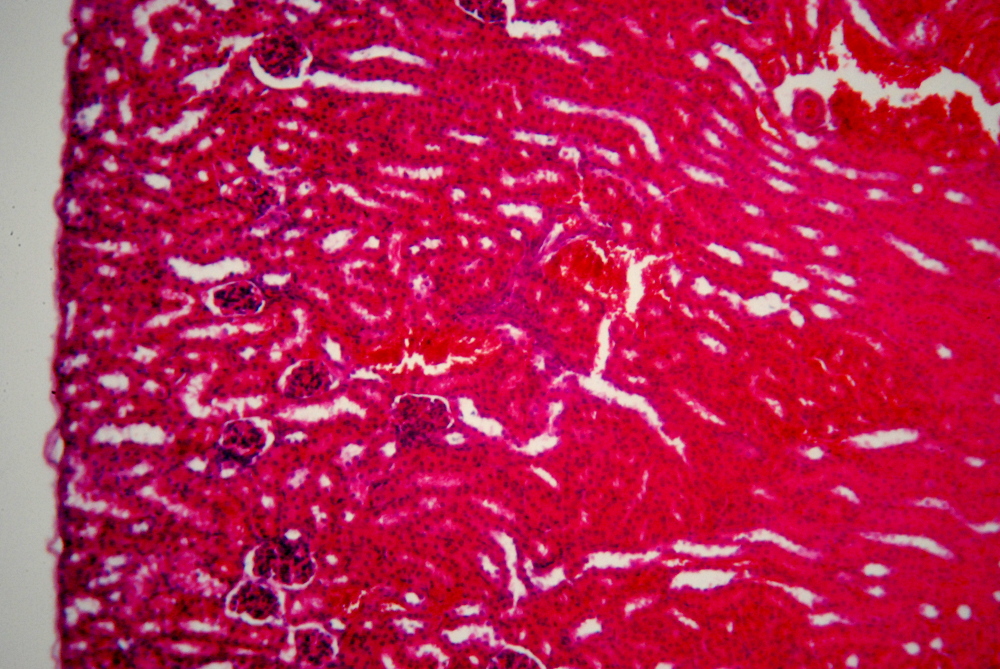
Use of the prescription heartburn drugs already has been linked to short-term kidney problems such as acute kidney injury and an inflammatory kidney disease called acute interstitial nephritis, Grams said.
Newer studies now show a link between the drugs and chronic kidney disease, in which the kidneys lose their ability to filter blood effectively.
Over time, chronic kidney disease can lead to kidney failure, forcing someone to undergo regular dialysis and possibly a kidney transplant, according to the U.S. National Institutes of Health.
In this new study, researchers used data on self-reported proton pump inhibitors use among more than 10,000 people taking part in a national study on hardening of the arteries. The researchers also evaluated data on outpatient PPI prescriptions among nearly 250,000 patients of a health care system in Pennsylvania.
From the start, PPI users in both groups were more likely to have health problems, such as obesity, high blood pressure and heart problems, the study noted.
In both groups, researchers associated use of the drugs with an increased risk of chronic kidney disease over 10 years.
The researchers also compared people using the drugs once a day with people who used them twice a day. They found twice-daily use was associated with a 46 percent increased risk of chronic kidney disease, versus a 15 percent increased risk in those taking one daily dose.
No one is sure how the drugs might damage the kidneys, but a couple of leading theories exist, Grams said. The medications can cause magnesium levels to decline in the body, and a lack of this important mineral could damage the kidneys. The kidneys also might become damaged over time if patients suffer repeated bouts of acute kidney inflammation due to proton pump inhibitors.
Gastroenterologists already are cautious regarding the use of the drugs, because they’ve been tied to other health problems such as bone fractures and infections of C. difficile and pneumonia, said Dr. Arun Swaminath, director of the inflammatory bowel disease program at Lenox Hill Hospital in New York City.
“We have started to limit the time you have to be on it, and limit the amount you take,” Swaminath said.
Because the new study isn’t a clinical trial, it doesn’t prove that PPI use causes chronic kidney disease, said Dr. Kenneth DeVault, president of the American College of Gastroenterology and chair of medicine at Mayo Clinic in Jacksonville, Fla.
“These types of studies, these big data studies, can sometimes suggest a signal that something’s going on, but I don’t know if they prove it,” DeVault said.
It’s possible that the drug users suffer chronic kidney disease more often because they have overall poorer health, he said.
Grams said the study authors tried to address that concern by comparing PPI users to people using another heartburn medication called H2 blockers. Both patient groups tended to be equally unhealthy, but PPI users had a 39 percent higher risk of chronic kidney disease, the researchers said.
While this study shouldn’t lead anyone to knee-jerk stop using proton pump inhibitors, people who use them regularly should talk with their doctor about whether they really need them, Grams and DeVault said.
“If you don’t need these medicines, you shouldn’t take them,” DeVault said. “That said, there are reflux patients with heartburn who really need the PPIs to help them with their symptoms.”
Doctors also might opt to prescribe an H2 blocker like Pepcid, Tagamet or Zantac. “To me, this is a cheaper, safer alternative that might work as well with some patients,” Swaminath said.
More information
For more on chronic kidney disease, visit the National Kidney Foundation.
Copyright © 2026 HealthDay. All rights reserved.