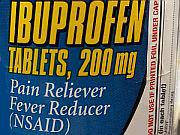
FRIDAY, July 10, 2015 (HealthDay News) — People who regularly reach for widely used painkillers like ibuprofen and naproxen may need to think carefully before they pop those pills, heart experts say.
Mounting evidence has shown that chronic use of non-steroidal anti-inflammatory drugs (NSAIDs) can raise a person’s risk of heart attack and stroke.
The evidence is strong enough that the U.S. Food and Drug Administration on Thursday ordered drug makers to toughen warning labels on both prescription and over-the-counter NSAIDs. The tougher warning does not include aspirin, an NSAID that has been shown to lower heart risks in some patients.
Most people who occasionally take ibuprofen (Advil, Motrin) or naproxen (Aleve) for infrequent headaches or pain don’t have to worry, as long as they follow the dosage directions on the bottle, said Dr. Richard Chazal, president-elect of the American College of Cardiology.
However, people who have existing heart problems or carry risk factors for heart disease need to carefully weigh the pain relief they’ll receive against a definite rise in their risk for heart attack or stroke, said Chazal, who’s also medical director of the Heart and Vascular Institute at Lee Memorial Health System in Fort Myers, Fla.
“These are the people who have to be particularly careful about using these medications,” he noted.
Doctors are also concerned about people with chronic pain problems who use NSAIDs on a regular basis, even if they have good heart health, said Dr. Mark Creager, president of the American Heart Association and director of vascular medicine at Brigham and Women’s Hospital in Boston.
“Even after just several weeks of use of an NSAID, the risk of heart attack or stroke goes up,” Creager said. “The risk is high with regular use, and it’s likely that the risk is greater when higher doses of these drugs are used.”
People who fall into these categories should talk with their doctor about their use of NSAIDs, to see if there are safer alternatives and to become more aware of their personal risk, experts said.
Studies estimate that a person’s relative risk of heart attack and stroke increases between 10 percent to 50 percent when they regularly take an NSAID, depending on the particular drug and the dose being used, according to the FDA.
What’s the connection? Researchers suspect that certain NSAIDs might alter the lining on the walls of blood vessels, increasing the risk of blood clots that can cause heart attacks or strokes, Chazal explained.
The current warning on NSAID packaging reads: “NSAIDs may cause an increased risk of serious heart thrombotic [clot] events, myocardial infarction [heart attack] and stroke, which can be fatal. Patients with heart disease or risk factors for heart disease may be at greater risk.”
The updated warning says: “NSAIDs cause an increased risk of serious heart thrombotic events, including myocardial infarction and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use.”
“They’ve removed the word ‘may,’ and the warning now also says that risk starts almost immediately,” FDA spokesman Eric Pahon said.
The FDA also is warning people who regularly use NSAIDs to be careful about using other products that might contain an NSAID, such as a multi-symptom cold product.
The FDA first added a boxed warning about heart risks to NSAID labels in 2005, after Merck & Co. pulled its popular painkiller Vioxx off the market.
Vioxx was a powerful NSAID from a class known as cox-2 inhibitors. Merck took Vioxx off the market in 2004 after a landmark study led by Cleveland Clinic cardiologist Dr. Steven Nissen linked the NSAID to a raised risk of heart attacks and strokes.
Drug company Pfizer has since hired Nissen to run a government-mandated clinical trial involving another controversial NSAID called Celebrex, a cox-2 inhibitor, which is still on the market. That trial is expected to wrap up next year, after enrolling more than 24,000 patients since 2007.
Nissen said it’s natural that consumers would be a little confused by the new FDA warning, “because the statement by the FDA is deliberately vague.”
Based on other studies and the findings from the Celebrex trial, Nissen said there is a suggestion of an increased risk of heart attack and stroke with these drugs, but that “the quality of the data leading to this recommendation is not particularly high.”
Still, people who need NSAIDs to treat their pain should continue to take them after consulting with their doctors, said Nissen, chair of heart medicine at the Cleveland Clinic.
“Pain is a terrible burden to bear. For people who have severe arthritis, we want people to understand they can take the drugs,” Nissen said. “There’s an increased risk, and they need to understand that, but we don’t want them to suffer the burden of pain with no relief.”
Chazal agreed that some people will need to continue using NSAIDs, but said that they still should work with their doctors to explore alternative medications and therapies.
People who do not have an affliction would do well to consider alternatives to NSAIDs, Chazal added. For example, people who take ibuprofen or naproxen to ease their aches following a strenuous workout should think instead about soaking in a hot tub or performing some flexibility exercises before or after they exercise.
“Getting in the habit of simply reaching for an NSAID without thinking about it is probably not in our best interest,” he said.
Finally, people who regularly use NSAIDs should understand that their baseline risk for heart disease also plays a factor in whether they should use these drugs, Creager said.
“NSAIDs will increase risk of heart attack, but when you balance benefit and risk you need to know what your starting risk is,” he said. “For example, risk in an older person or a person who already has had a heart attack is going to be greater than risk in a younger person. Understand where on that scale you sit.”
More information
To learn more about the new NSAID warning, visit the Food and Drug Administration.
Copyright © 2026 HealthDay. All rights reserved.