THURSDAY, June 13 (HealthDay News) — For the first time, researchers have shown that implanting electrodes in the brain’s “feeding center” can be safely done — in a bid to develop a new treatment option for severely obese people who fail to shed pounds even after weight-loss surgery.
In a preliminary study with three patients, researchers found that they could safely use the therapy, known as deep brain stimulation (DBS). Over almost three years, none of the patients had any serious side effects, and two even lost some weight — but it was temporary.
“The first thing we needed to do was to see if this is safe,” said lead researcher Dr. Donald Whiting, vice chairman of neurosurgery at Allegheny General Hospital in Pittsburgh. “We’re at the point now where it looks like it is.”
The study, reported in the Journal of Neurosurgery and at a meeting this week of the International Neuromodulation Society in Berlin, Germany, was not meant to test effectiveness.
So the big remaining question is, can deep brain stimulation actually promote lasting weight loss?
“Nobody should get the idea that this has been shown to be effective,” Whiting said. “This is not something you can go ask your doctor about.”
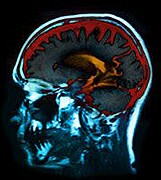
Right now, deep brain stimulation is sometimes used for tough-to-treat cases of Parkinson’s disease, a movement disorder that causes tremors, stiff muscles, and balance and coordination problems. A surgeon implants electrodes into specific movement-related areas of the brain, then attaches those electrodes to a neurostimulator placed under the skin near the collarbone.
The neurostimulator continually sends tiny electrical pulses to the brain, which in turn interferes with the abnormal activity that causes tremors and other symptoms.
What does that have to do with obesity? In theory, Whiting explained, deep brain stimulation might be able to “override” brain signaling involved in eating, metabolism or feelings of fullness. Research in animals has shown that electrical stimulation of a particular area of the brain — the lateral hypothalamic area — can spur weight loss even if calorie intake stays the same.
The new study marks the first time that deep brain stimulation has been tried in that brain region. And it’s an important first step to show that not only could these three severely obese people get through the surgery, but they also seemed to have no serious effects from the brain stimulation, said Dr. Casey Halpern, a neurosurgeon at the University of Pennsylvania who was not involved in the research.
“That shows us this is a therapy that should be studied further in a larger trial,” said Halpern, who has done animal research exploring the idea of using deep brain stimulation for obesity.
“Obesity is a major problem,” Halpern said, “and current therapies, even gastric bypass surgery, don’t always work. There is a medical need for new therapies.”
The three patients in Whiting’s study were examples of that medical need. All were severely obese and had failed to shed weight after gastric bypass surgery — the current last-ditch treatment option.
During the study period, the patients did have some side effects from deep brain stimulation — nausea, anxiety and feeling “too hot or flushed” — but they were short-lived, the researchers said. And there was some evidence that the brain stimulation was having effects. In lab tests, Whiting’s team found that the deep brain stimulation seemed to spur short-lived spikes in resting metabolism.
Then, after the deep brain stimulation was programmed to the settings that seemed to boost metabolism, two patients shed some pounds — 12 percent to 16 percent of what they weighed before the DBS settings were “optimized.”
“There was some weight loss, but it was transient,” Whiting said. Now a key question is, what is the right setting for the deep brain stimulation to encourage lasting weight loss? Whiting said his team is continuing to follow these three patients to try to figure that out — and to keep monitoring safety.
Although deep brain stimulation is considered a generally safe therapy for the right patients, it is a major undertaking that requires two surgeries — one to implant electrodes in the brain and another to place the neurostimulator. The potential risks include infection, a blood clot or bleeding in the brain, or an allergic reaction to the DBS parts.
If deep brain stimulation ever does become an option for managing severe obesity, Whiting said, he would expect it only to be used when all else fails. “This would definitely be a last resort,” he said.
“At first, it would absolutely be a last-ditch option,” neurosurgeon Halpern said. But, he added, it’s also possible that deep brain stimulation could become an add-on therapy, used after gastric bypass for some patients whose weight does not fall — or even an alternative in certain cases where bypass surgery is too risky.
Medtronic provided the deep brain stimulation hardware for the study and funded the work. One of Whiting’s co-researchers is employed by the company.
More information
Learn more about brain stimulation therapies from the U.S. National Institute of Mental Health.