WEDNESDAY, June 29 (HealthDay News) — In 2009, a 60-year-old American lab researcher was mysteriously, and fatally, infected with the black plague while conducting experiments using a weakened, non-virulent strain of the microbe.
Now, a follow-up investigation has confirmed that the researcher died because of a genetic predisposition that made him vulnerable to the hazards of such bacterial contact.
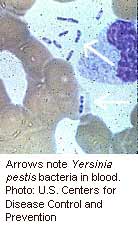
The new report appears to set aside fears that the strain of plague in question (known by its scientific name as “Yersinia pestis”) had unpredictably mutated into a more lethal one that might have circumvented standard research lab security measures.
“This was a very isolated incident,” said study co-author Dr. Karen Frank, director of clinical microbiology and immunology laboratories in the department of pathology at the University of Chicago Medical Center. “But the important point is that all levels of public health were mobilized to investigate this case as soon as it occurred.
“And what we now know,” Frank added, “is that, despite concerns that we might have had a non-virulent strain of virus that unexpectedly modified and became virulent, that is not what happened. This was an instance of a person with a specific genetic condition that caused him to be particularly susceptible to infection. And what that means is that the precautions that are typically taken for handling this type of a-virulent strain in a lab setting are safe and sufficient.”
Frank and her UC colleague, Dr. Olaf Schneewind, reported on the case in the June 30 issue of the New England Journal of Medicine.
According to the National Institutes of Health, prairie dogs, rats and other rodents, and the fleas that bite them, are the principle carriers of the bacteria responsible for the spread of the deadly plague, and they can infect people through bites.
In the 1300s, the so-called “Black Death” claimed the lives of more than 30 million Europeans (about one-third of the continent’s total population at the time). In the 1800s, 12 million Chinese died from the illness. Today, only 10 to 20 Americans are infected yearly.
As first reported by the U.S. Centers for Disease Control and Prevention on Feb. 25, the case of the American lab researcher began in September 2009, when he sought care at a hospital emergency room following several days of breathing difficulties, dry coughing, fevers, chills, and weakness. Thirteen hours after admission, he was dead.
An autopsy and blood tests showed that the man had an underlying blood disorder called hemochromatosis, which involves harboring too much iron, according to the CDC report. The strain of the microbe he was working with in the lab was weak because it didn’t have enough iron. But once the bacteria entered his body, his extra iron might have been enough to overcome the bacteria’s weakness, rendering it as virulent as some of its cousins.
The case was the first since 1959 involving plague transmission in a laboratory setting — and it remains unclear exactly how the virus entered the lab researcher’s body. It was also the first ever to be linked to a weakened plague strain that had not been considered a threat to human health.
The strain was thought to be so safe that it was routinely used as a subject for basic scientific research. Such experiments are typically conducted under relatively moderate security conditions, compared with those in place when researchers are in contact with highly communicable diseases.
In the new report, the investigators emphasized the need for vigilance in following lab safety protocols and suggested that researchers consider testing for the hemochromatosis mutation before coming into contact with Y. pestis.
Dr. Steven Hinrichs, chairman of the department of pathology and microbiology at the University of Nebraska Medical Center in Omaha, noted that genetic research advances now allow investigators to rapidly assess epidemiological concerns in such cases.
“Our ability to investigate this kind of situation, and perform the genetic tests that identify the underlying susceptibility of an individual, would not have been possible even a few years ago,” he said.
“In fact, just a few years ago we might have been very, very concerned about this,” Hinrichs said. “But because we could actually genotype this individual and prove that he had this mutation, the explanation for this outcome is totally acceptable and understandable.”
More information
For more on the plague, visit the U.S. National Institutes of Health.

