SUNDAY, June 10 (HealthDay News) — Progress continues to be made on the development of an artificial pancreas, a device that would ease the burden of living with type 1 diabetes.
Several artificial pancreas research groups presented their latest findings Saturday at the American Diabetes Association annual meeting in Philadelphia, and the hope is that the makers of one or more of the devices will be seeking regulatory approval within the next five years.
“I’m cautiously optimistic,” said Aaron Kowalski, assistant vice president for treatment therapies at the Juvenile Diabetes Research Foundation. “The FDA has really turned the corner and is moving much faster…. My hope is that in the next year or two, we’ll see approvals on devices that can minimize [low blood sugar levels], and that’s just the tip of the iceberg.”
Type 1 diabetes is an autoimmune disease in which the body’s immune system turns against healthy cells. In type 1 diabetes, the immune system attacks beta cells in the pancreas, effectively destroying the body’s ability to produce the hormone insulin. Insulin helps metabolize carbohydrates from food and fuels the body’s cells.
Type 1 diabetes can be managed with insulin injections or a pump that delivers insulin via a tiny catheter inserted under the skin every few days. The problem with both insulin-delivery techniques is that people have to estimate how much insulin they’ll need based on the foods they eat and how much activity they will be doing.
Too much insulin can result in low blood sugar levels (hypoglycemia), which, in turn, can cause a person to pass out. Low blood sugar levels can even lead to death. Too little insulin leads to high blood sugar levels (hyperglycemia), which over time can cause serious complications, such as heart disease and kidney and eye problems.
An artificial pancreas, which sometimes is referred to as a closed-loop system because it doesn’t require user input, could potentially solve those problems by taking over the decision-making process and applying sophisticated computer algorithms to decide how much insulin is needed at any given moment.
But developing such a device isn’t as easy as it sounds.
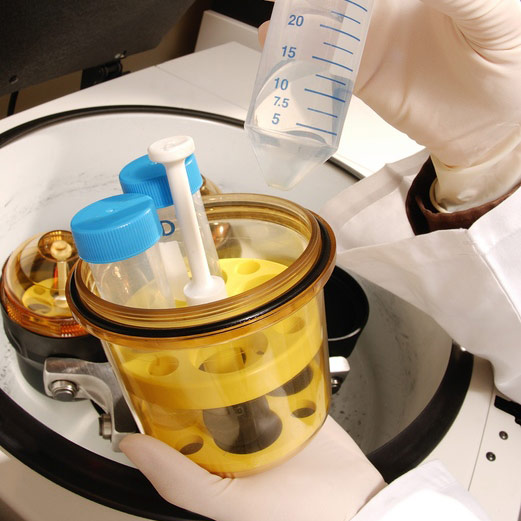
First, the device has to be able to continuously detect patients’ blood sugar levels and know whether the levels are trending up or down. There has to be a piece of the device that holds and delivers insulin. And there needs to be a way to deal with low blood sugar levels.
Someone with type 1 diabetes typically consumes food or a sugar-containing drink to counteract drops in blood sugar. Some devices will shut off and sound an alarm to alert the person to treat their low blood sugar.
At least one device in development contains not only insulin, but also a hormone called glucagon that can quickly raise blood sugar levels.
Researchers at Boston University, Harvard Medical School and Massachusetts General Hospital are developing the device. In addition to reporting on the latest in-hospital trials of their device, they presented a prototype that uses a continuous glucose monitor, an insulin pump that also will house the artificial pancreas software with a low-powered Bluetooth device, and an app designed for the iPhone 4S, said Edward Damiano, one of the device’s developers.
“It’s a totally pocket-sized device,” said Damiano, associate professor of biomedical engineering at Boston University. Damiano, who will be wearing his team’s version of the artificial pancreas for the presentation, said their device is the only one that truly is closed-loop because it includes both glucagon and insulin, allowing it to respond to both high and low blood sugar levels without user input.
Damiano said they soon will be filing paperwork for five-day in-hospital trials of their system. They also are planning two transitional studies for summer 2013 that will include campers at a diabetes camp and hospital personnel with type 1 diabetes. If all goes well, their hope is that they will be able to do a large-scale six-month outpatient trial by 2015, Damiano said.
Another research group, at the University of Virginia School of Medicine, is recruiting people for outpatient trials on an artificial pancreas device similar to the one Damiano’s team is working on. Although this device also uses a smartphone to display the device’s information, however, it contains only insulin, not glucagon.
Another device, called a Hypoglycemia-Hyperglycemia Minimizer, which was developed in a partnership with the Juvenile Diabetes Research Foundation and the insulin-pump maker Animas, was able to automatically predict increases and decreases in blood sugar levels. It also was able to change insulin delivery accordingly in a study that included 13 people between 24 and 57 years old with type 1 diabetes.
“The successful completion of this study using the [Hypoglycemia-Hyperglycemia Minimizer] system in a human clinical trial is a significant step forward in the development of an advanced first-generation artificial pancreas,” Dr. Henry Anhalt, chief medical officer for Animas, said in a statement.
Kowalski is optimistic about the future development of an artificial pancreas.
“This gives me a lot of hope that we’re really starting to roll to what could be full-blown product development,” he said.
Kowalski said he believes the artificial pancreas likely will be approved in steps. “I don’t think it will be one product, but an evolution,” he said.
First, he said, will be a device designed to minimize the impact of severe low blood sugar. After that, it’s likely that there will be a device to prevent low blood sugar from occurring in the first place.
“Each of these steps should be meaningful, make life easier and improve glucose control for people with type 1 diabetes,” Kowalski said.
More information
Learn more about the artificial pancreas from the U.S. Food and Drug Administration.