MONDAY, Feb. 18 (HealthDay News) — Doctors often don’t discuss the psychological impact and long-term risks of implantable cardioverter defibrillators (ICDs) with their patients. This leaves people unaware of how seriously the devices can affect their quality of life, a new study finds.
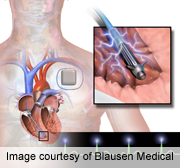
Patients have this device implanted in their chest or abdomen to treat arrhythmia — an abnormal heartbeat. The ICD provides electrical shocks to restore a normal heartbeat and prevent fatal cardiac arrest.
“Getting an ICD is clearly a life-changing event for the patient,” study principal investigator Dr. Paul Hauptman, a professor of internal medicine at the Saint Louis University School of Medicine, said in a university news release. “Physicians not only have to point out the benefits of this device, but also let the patients know about its risks beyond those of the implantation procedure itself.”
The study involved 41 patients with ICDs and 11 cardiologists in three cities. The participants provided details on the discussions they had with their doctors before their ICD was implanted.
After receiving an ICD, many of the patients experienced symptoms of depression, anxiety and changes in their body image. They said these possible side effects were not mentioned in discussions they had with their doctor before the procedure.
Also after receiving the device, many patients had trouble performing routine physical labor. Others reported that they did not like air travel due to extra security screening at airports.
Eighty percent of patients said they did not discuss any possible long-term complications from an ICD with their doctor before the procedure. These patients also reported that they were not warned about any changes they could expect in their quality of life.
In conducting the study, the researchers also observed cardiologists informing “fake” patients about getting an ICD. The doctors focused on the device itself, and not how it would affect their patients.
“We were interested in how physicians communicate with patients and explain the impact of an expensive, invasive technology on quality of life,” study co-principal investigator, Eric Armbrecht, director of consulting practice at Saint Louis University Center for Outcomes Research, explained in the news release. “This study revealed physicians talked more about the technology of the device instead of communicating the expectations patients should have from it.”
Most study patients initially thought the ICD would provide a cure for their condition, but later realized that wasn’t true.
“Patients reported that their physicians described the device as a safety net, calling it absolutely necessary. We found that many patients end up having unrealistic expectations of what the technology is going to do for them,” Armbrecht said. “For moral, ethical and economic reasons, patients need to be equipped to make informed decisions about their own health.”
The authors noted that some patients without a history of cardiac arrest or arrhythmia symptoms receive an ICD as part of a primary prevention strategy even though the device can lead to side effects, such as anxiety and depression. ICDs may also have mechanical defects, which could require additional procedures to replace parts.
Patients who have experienced a life-threatening arrhythmia benefit more from receiving an ICD as part of a secondary prevention strategy, according to the researchers.
“Seven to eight patients out of 100 will accrue a survival benefit when the ICD is implanted for primary rather than secondary prevention. The majority will not gain a survival benefit over standard of care,” noted Hauptman. “Unfortunately, the screening methodology used to identify patients who are at risk of sudden death is not very good.”
Doctors need a better way to communicate with their patients, the researchers concluded. “Physicians need tools and resources so they can counsel patients about ICDs in a more systematic, judicious and transparent manner,” Armbrecht said.
And, Hauptman added, “Cardiologists need to be trained in communication with patients that will promote informed decision making and preempt threats to patient quality of life.”
The study was published online Feb. 18 in JAMA Internal Medicine.
More information
The U.S. National Heart, Lung, and Blood Institute has more about implantable cardioverter defibrillators.

