WEDNESDAY, June 13 (HealthDay News) — A woman with early-stage lung cancer died recently after highly targeted radiation therapy zapped not just her tumor, but surrounding tissue, fatally damaging her airway.
Though just a single case report of an apparently deadly complication, the authors warn that targeted radiation therapy — specifically, stereotactic body-radiation therapy — has inherent risks, even when done properly and using an even lower dose of radiation than is considered safe.
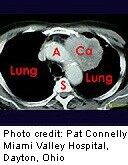
Stereotactic body-radiation therapy focuses beams of radiation on a tumor in the hopes of killing it. Because it uses highly precise beams that can focus large doses of radiation with millimeter accuracy, the technique is considered an advance over older types of radiation therapy, which are generally more diffuse, explained Dr. Len Lichtenfeld, deputy chief medical officer for the American Cancer Society. The goal is to reduce exposure of healthy tissue to the radiation to avoid side effects, while more effectively shrinking the tumor with the higher doses of radiation delivered over a shorter period of time.
Stereotactic radiation is increasingly used to treat early-stage lung cancer. Though the first choice of treatment for early-stage lung cancer is surgery, radiation is turned to in people who cannot withstand having a portion of their lung removed because of other health issues, such as serious underlying heart or lung disease, said Dr. Ramesh Rengan, an assistant professor of radiation oncology at University of Pennsylvania Perelman School of Medicine.
Rengan wrote the case report published in the June 14 issue of the New England Journal of Medicine.
In the case report, a 61-year-old woman with a history of smoking and stage 1 adenocarcinoma — meaning the two tumors were small and had not spread to the lymph nodes or other organs — was treated, seemingly successfully, with stereotactic body radiation. Adenocarcinoma is a common type of non-small cell lung cancer.
But eight months later, not only did the woman have new metastases (spread of the cancer), a bronchoscopy — a camera threaded into the airway — showed an “extensive area of necrosis,” or dead tissue, near the radiated area.
Her physicians at University of Pennsylvania did not do additional radiation. Instead, she underwent more chemotherapy, but began coughing up blood and died a few months later.
Researchers warned that patients with tumors near “radiation-sensitive” body parts, or body parts easily damaged by radiation relative to the dose needed to treat the cancer, such as the large airways, large blood vessels, the heart, certain nerves and the spinal cord, “may be at increased risk for severe radiation injury.”
“The reason why it’s so important to get this message out is because these side effects don’t manifest themselves immediately. They can take months to show up,” Rengan said. “And you will only find them if you are looking. Most patients aren’t undergoing bronchoscopy just for the heck of it. On a CT scan, the airway looks fine.”
Rengan urged physicians who use stereotactic radiation to follow patients carefully. Furthermore, the levels of radiation that are considered safe may need to be rethought, he added.
“This was a dose level that was previously believed to be safe for this type of tumor in this location,” he said.
Lichtenfeld praised the authors for writing the case report. Although one report does not have the weight of a clinical trial involving multiple patients from multiple institutions, anecdotal reports such as this can help raise awareness about the potential complications of a treatment that’s increasingly popular.
“Even though the doctors gave the radiation properly, they still got a serious complication,” Lichtenfeld said. “What this report is saying is even though we did this the right way, doctors and patients still need to be aware you can have bad effects from this type of radiation used in this way.”
More information
The U.S. National Cancer Institute has more on lung cancer.