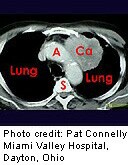
WEDNESDAY, Sept. 4 (HealthDay News) — Annual lung cancer screenings using low-dose CT scans can successfully detect malignant tumors before they can spread to other parts of the body, according to two new studies.
Yearly screenings with CT scans are more effective than regular chest X-rays in finding early stage cancers, according to a U.S. study that is part of the federally funded National Lung Screening Trial.
CT scans caught more early stage lung cancers than chest X-rays did during annual screenings over three years, the research team reported. What’s more, the ability to accurately detect cancer improved year to year.
“When we’re screening once a year every year we are finding early stage lung cancers that are potentially curable,” said Dr. Caroline Chiles, a professor of radiology in the Comprehensive Cancer Center of Wake Forest Baptist Medical Center and a principal investigator for the national lung screening study. “We really start seeing benefit when someone stays in annual screening.”
The findings appear in the Sept. 5 issue of the New England Journal of Medicine, along with another related study.
Canadian researchers have developed an effective method for sorting potentially dangerous tumors from benign nodules detected during a CT lung screening, the second study reports.
Their checklist takes into account the size, shape and location of detected nodules, as well as other risk factors such as smoking or family history, said lead author Dr. Stephen Lam, chair of the Provincial Lung Tumor Group and director of the MDS-Rix Early Lung Cancer Detection and Translational Research Program at the British Columbia Cancer Agency.
“Our nodule predictor has an accuracy of over 90 percent in determining whether a nodule needs to be followed up to rule out a cancerous lesion,” Lam said.
Doctors using the checklist can prevent people from receiving unnecessary follow-up CT scans or biopsies, reducing their radiation exposure or surgical risk, said Lam, who is also a professor of medicine at the University of British Columbia.
These studies appear as U.S. officials are weighing whether to green-light annual CT scans as a preventive health measure for a specifically defined set of heavy smokers.
The U.S. Preventive Services Task Force — an independent volunteer panel of national health experts — has recommended regular low-dose screenings for current and former smokers aged 55 to 80 with at least a 30 “pack-year” history of smoking who have had a cigarette sometime within the last 15 years.
Pack years are determined by multiplying the number of packs smoked daily by the number of years a person has smoked. For example, a person who has smoked two packs a day for 15 years has 30 pack years, as has a person who has smoked a pack a day for 30 years.
A public comment period on the task force’s draft recommendation ended on Aug. 26. The health care community now awaits the panel’s final rule.
The U.S. study follows up on earlier findings that showed that three years of low-dose CT scans reduced lung cancer deaths by about 20 percent. The trial involved more than 53,000 people who were assigned either CT scans or chest X-rays for three years.
The new study provides more detail on how the follow-up annual scans improve the effectiveness of screening, Chiles said.
“You have to show not only an increase in the number of patients with early stage, you also have to show a decrease in the number of advanced-stage lung cancer,” Chiles said. “That way, we know the true benefit comes with the screenings that come in the following year, and the year after that. Cancer was not detectable the year earlier.”
Early stage lung cancer accounted for about half of the cancers detected by CT scans in the first and second follow-up years. Only 24 percent of the cancers detected by chest X-rays were early stage.
At the same time, CT scans detected half as many cancers that had been allowed to progress to the last stage: 15 percent of all cancers detected, compared with 30 percent of all the cancers detected by X-rays.
“We saw a significant decrease in the number of late-stage lung cancers,” Chiles said. “We feel we showed a shift to early stage treatable lung cancer in the low-dose CT group.”
The Canadian researchers took a similar multiyear tack. They used their checklist to assess the potential hazard of lung nodules detected during the first CT scans, and then used two years of follow-up lung screenings to see whether their model worked.
A total of more than 12,000 lung cancer nodules observed on CTs of nearly 3,000 current and former smokers were examined.
The checklist runs counter to current standards, which mainly rely on the size of a nodule to determine whether more tests should be run.
But the team found that in one of five study participants, the largest nodule in their lungs did not prove malignant. Other dynamics like the shape of the mass, its location in the lung, and the individual person’s risk factor must be accounted for to properly assess the hazard posed.
For example, nodules located in the upper lobes of the lungs increased the likelihood of cancer, the report says. However, more nodules found in a CT scan actually decreases cancer risk.
The new model is much better at predicting cancer than previous checklists, said Dr. Christine Berg, co-principal investigator of the National Lung Screening Trial for the U.S. National Cancer Institute.
“If you have a nodule you can predict it’s positive almost 20 percent, which is a lot better than what we had,” she said.
The model is even better at ruling out nonmalignant nodules, which could save patients from unnecessary repeat testing, lowering their radiation exposure and risk from procedures.
“If you say something is benign using the model, the chances of it being malignant are extremely small, about 99.6 percent,” Berg said. “This is an excellent first cut of determining whether a nodule on your scan is malignant or not.”
More information
For more information on lung cancer screening, visit the U.S. National Cancer Institute.
Copyright © 2026 HealthDay. All rights reserved.