MONDAY, April 9 (HealthDay News) — Screening people at high risk for lung cancer could be at least as cost-effective as screening for breast, colorectal and cervical cancers, a new study suggests.
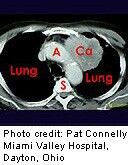
A group of actuaries specializing in the health care industry estimated how much private insurance companies would pay and the survival benefits that would follow if they covered lung cancer screening. They based their study on using a scanning technology called low-dose spiral computed tomography (CT) on people between the ages of 50 and 64 who were at high risk for developing lung cancer due to their smoking history.
The authors estimated that screening high-risk people would cost providers less than $19,000 for every year of life saved. The study was published in the April issue of Health Affairs.
In comparison, the costs per life-year saved for breast, colorectal and cervical cancer screening — the three types of screening that have widespread support in the United States — are at least about $31,000, $19,000 and $50,000, respectively, according to the authors, who updated estimates from previous analyses.
The authors also estimated that insurance rates would increase by 76 cents per month if half of the eligible members got screening.
“[Lung cancer] is a very deadly kind of cancer, but it is also concentrated in a relatively small group of people who have a history of smoking. That’s why the economics makes such powerful sense here,” said study author Bruce Pyenson, a principal and consulting actuary at Milliman, based in New York City.
About 220,000 people will be diagnosed with lung cancer and 160,000 will die from the disease in 2012, according to the American Cancer Society. The five-year survival rate after diagnosis is only about 16 percent, in part because most people have advanced lung cancer by the time they are diagnosed.
Most health organizations do not recommend lung cancer screening, or testing people before they have symptoms. The U.S. Preventive Services Task Force (USPSTF) does not support CT scan, chest X-rays or sputum cytology, in which mucus from the lungs is examined, because it states that there is not enough evidence that these tests reduce the number of lung cancer deaths.
On the other hand, lung cancer screening can detect benign tumors, leading to unnecessary invasive biopsies, and increases radiation exposure.
The USPSTF guidelines are probably the “single most important factor” for Medicare and private insurance companies in deciding whether or not to cover lung cancer screening, said Dr. William Black, a radiologist at Dartmouth-Hitchcock Medical Center in Lebanon, N.H.
And while neither the USPSTF nor insurance companies base their guidelines or coverage on costs, the USPSTF often looks at proxies to cost like the number of people needed to treat to have a certain effect, Black explained.
“Although in the past [cost] has not been a criteria for Medicare, many people expect that to change,” Pyenson said. “Expenditure in health care overall is not sustainable.”
In addition to the current study suggesting the cost-effectiveness of lung cancer screening, recent support for screening came in 2011 when results of the National Lung Screening Trial (NLST) were published. It found that getting CT scans every year for three years reduced lung cancer deaths by 20 percent compared with chest X-rays in current or former smokers between 55 and 74 years of age.
“I think it’s certainly possible the USPSTF will endorse it, but if they did they would definitely restrict it to people like in the NLST,” Black said, adding that he expects that the Task Force will update its guidelines sometime in 2013.
The current study simulated the effect of annual CT scans in people between 50 and 64 who had smoked at least a pack of cigarettes a day for 30 years. The group did not include people older than 64 because that is when Medicare kicks in and it would be more difficult to determine the cost to private insurers, Pyenson explained. The research was funded by the Lung Cancer Alliance and the American Legacy Foundation.
Pyenson and his colleagues estimated the number of deaths associated with early and late stages of lung cancer over a 15-year period (to reflect the 15 years between ages 50 and 64).
To estimate the number of life-years saved by lung cancer screening, the group used data collected from lung cancer screening programs to predict at what stage lung cancers would have been detected if screening had been in place and as a result how many fewer lung cancer deaths there would have been.
Although the authors concluded that cost-benefit ratio for lung cancer screening is relatively low, one expert suggested they might be underestimating the total cost.
“I can’t imagine how it could be that low,” said Pamela McMahon, associate director of the Massachusetts General Hospital Institute for Technology Assessment in Boston.
In a 2011 study, McMahon and her colleagues estimated that annual CT screening for people between 50 and 74 who had smoked at least one pack a day for 20 years would cost between $126,000 and $169,000 for every quality-adjusted life-year.
One important difference with McMahon’s analysis is that her group considered all costs associated with screening, such as how much a patient would spend to travel to the clinic once a year for screening. “I would imagine this cost is going to be pretty different,” McMahon said.
Nonetheless, McMahon thinks that lung cancer screening will eventually be adopted in the United States. “Whether it will be as inexpensive as $19,000 or as expensive as we estimated remains to be seen,” she noted.
In addition, McMahon’s study found that the cost effectiveness got a boost when screening had an effect on smoking quit rates. If getting screened doubled quit rates, the cost effectiveness for a 50-year-old who smoked a pack a day for 20 years was $75,000 per quality-adjusted life-year.
“I think that smoking cessation programs should definitely be part of whatever screening programs get adopted,” McMahon said.
More information
To learn more about lung cancer and screening, visit the American Cancer Society.