WEDNESDAY, April 15, 2015 (HealthDay News) — If genetic tests are only done on cancer tissue, as many as half of patients may not receive the most appropriate treatment for their cancer, a new study reports.
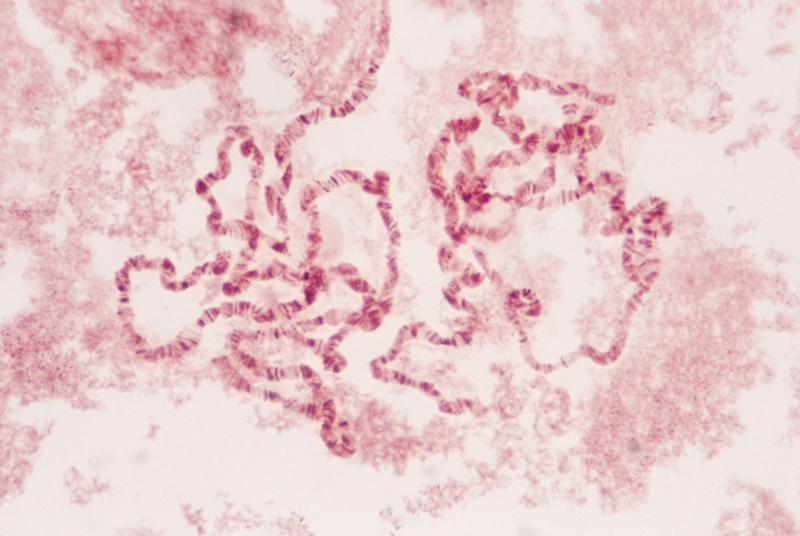
Cancer doctors increasingly rely on genetic testing to look for opportunities to use treatments that target specific genetic causes of cancer — called targeted therapy.
But doctors often examine just the genetics — or DNA — of a patient’s cancerous tissue, and don’t compare it against a genetic analysis of normal tissue, explained study senior author Dr. Victor Velculescu. He is a professor of oncology and pathology at Johns Hopkins University School of Medicine, and co-director of the school’s Cancer Biology Program.
The problem is that it’s not unusual for people to have genetic variations in normal tissue that aren’t causing cancer. By ignoring a person’s normal genetics and only looking at the genetics of the cancer, doctors can be fooled by those normal variations and assume that these harmless mutations are the cause of the patient’s cancer, the researchers found.
Their findings show that unless doctors compare the DNA of cancerous tissue to normal tissue, they run the risk of misjudging the genetic causes of a person’s cancer about half the time.
“These false positive changes affected roughly one in every two patients analyzed,” said Velculescu. “In other words, one in two patients receiving tumor-only gene panel sequencing is potentially at risk to receive a treatment that may be inappropriate.”
Treatments based on the wrong genetic diagnosis could range from merely ineffective to potentially harmful, and all at a great financial cost, Velculescu said. Targeted cancer therapies are some of the most expensive medications on the market, and can have very severe side effects, he added.
The study was published April 15 in the journal Science Translational Medicine.
For the study, the researchers compared the genetic information of tumor and normal tissue from 815 patients. These patients had a variety of cancers, including breast, brain, renal, gastric, lung, pancreatic, and blood cancers and melanoma.
Three-quarters of patients had genetic mutations for which approved therapies or clinical trials had been designed, suggesting that DNA analysis could steer these people to targeted therapy, Velculescu said.
However, a comparison of cancerous and normal tissue found that about two-thirds of all the mutations uncovered by DNA scans “were a part of the patient’s normal inherited genetic variation,” he said. “In other words, they were false positives.”
The researchers then looked specifically at mutations in genes for which some kind of drug or cancer therapy has already been identified.
They found that nearly a third of these changes also were false positives — harmless genetic variations that had nothing to do with a person’s cancer.
Each patient had multiple harmless genetic mutations, according to Velculescu. Overall, he said, the false positives affected almost one in every two patients.
Based on these findings, the researchers argued that doctors should begin obtaining DNA analysis of both normal and cancer tissue from patients. That would allow doctors to screen out normal genetic variations and more accurately determine the causes of a person’s cancer.
“Of course we all want precision medicine, but one conclusion from these analyses is that we cannot have precision medicine without precision genomics,” Velculescu said. “We can’t expect physicians to provide the right therapy to the right patients if we can’t obtain accurate results in our diagnostic tests.”
Angela Colmone, associate editor of Science Translational Medicine, agreed.
“These findings suggest that sequencing paired tumor and normal samples would yield more accurate diagnosis and treatment plans than the current standard methods,” Colmone said.
Velculescu said such a change in procedure could be done almost immediately, after some hurdles are passed.
At this time, insurance companies don’t cover the cost of such additional sequencing, he said.
“There is an additional cost to this type of analysis, but I think it is not double the cost of the initial test, because less sequencing needs to be done for the normal specimen,” Velculescu said.
In addition, hospitals and clinics would have to change their procedures so that normal tissue samples are gathered at the same time as cancerous tissue samples. Velculescu suggested that a saliva sample likely could do the trick, and avoid the need to draw blood from the patient.
More information
For more information on targeted cancer therapies and genetics, visit the U.S. National Institutes of Health.
Copyright © 2026 HealthDay. All rights reserved.