TUESDAY, June 11 (HealthDay News) — Newer, costlier treatment for rheumatoid arthritis appears no better than an older, less-expensive regimen for people who don’t respond to the first-line drug methotrexate, a new study suggests.
“Newer isn’t always better,” said researcher Dr. Ted Mikuls, an associate professor in the rheumatology division at the University of Nebraska Medical Center, in Omaha. “Some of the older medications can be effective.”
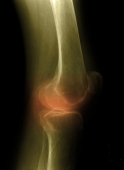
Rheumatoid arthritis causes inflammation in the joints, resulting in swelling, stiffness, pain and reduced joint function. It can also affect other parts of the body.
“We compared two different ways of treating rheumatoid arthritis — one that included a new biologic [medication] with an older, more conventional oral medication,” Mikuls explained. “We basically showed that at the end of the day patients, regardless of what they got, looked very similar in terms of pretty much every outcome we looked at in the study.”
Patients whose arthritis didn’t respond to methotrexate alone who were then given a combination of methotrexate, sulfasalazine (Azulfidine) and hydroxychloroquine (Plaquenil) did as well as patients given methotrexate and the new biologic drug etanercept (Enbrel) — which is given by injection — the researchers said.
“The treatments are very different in terms of costs,” Mikuls said. If a patient had to pay out of pocket for etanercept it could cost around $20,000 a year, while the out-of-pocket costs for the other drugs is a few hundred to a few thousand dollars, he said.
The out-of-pocket cost of etanercept varies by insurance provider, including those covering the Medicare drug benefit program, Mikuls added.
The report was published online June 11 in the New England Journal of Medicine to coincide with presentation of the study at the Annual European Congress of Rheumatology meeting in Madrid, Spain.
“This study addresses a real-life scenario for rheumatologists where patients are often on methotrexate and are not doing well and the question is what to do next,” said Dr. Soumya Reddy, an assistant professor in the rheumatology division of the dermatology department at NYU Langone Medical Center, in New York City.
About 20 percent to 40 percent of patients don’t respond methotrexate or can’t take the drug either because of side effects or it is not indicated for them, said Reddy, who was not involved in the study.
The findings are “reassuring,” in that when a biologic is not an option, due to cost or other reasons, the older regimen is effective, she said.
Which regimen is best really needs to be tailored to each patient, Reddy said.
For the study, researchers randomly assigned 353 patients to methotrexate, sulfasalazine and hydroxychloroquine or to methotrexate and etanercept for 48 weeks. Some patients switched from one regimen to another midway through the study.
The researchers found that both groups improved significantly, with no difference between the two treatments.
In addition, improvements in both groups were similar with regard to pain, quality of life, progression of their arthritis as seen on X-rays or side effects of the drugs.
For her part, Dr. Diane Horowitz, a rheumatologist at North Shore University Hospital, in Manhasset, N.Y., said the trial wasn’t long enough to really tell if treatment with etanercept is equal to the three-drug regimen.
“In other studies, people on biologics did better over the long term,” said Horowitz, who is also with the LIJ Medical Center, in New Hyde Park, N.Y. “I want to see more long-term data.”
For patients who don’t do well on methotrexate alone “there is some significant evidence that doing methotrexate plus sulfasalazine plus hydroxychloroquine [gives] a good response, and you don’t always have to jump to a biologic right away,” she said.
More information
To learn more about rheumatoid arthritis, visit the U.S. National Library of Medicine.

