THURSDAY, Feb. 9 (HealthDay News) — A shocking new national survey suggests that nearly all orthopedic surgeons may order unnecessary tests, referrals or hospitalizations to avoid being sued, to the tune of $2 billion a year.
The report is the first of its kind to demonstrate that “defensive medicine” — practiced to help exonerate doctors from malpractice accusations but adding no benefits to patient care — is common among orthopedic surgeons across the United States, the study authors said.
“All across America, orthopedic surgeons are moving away from a standard of care and doing things out of fear of lawsuits,” said study co-author Dr. Manish Sethi, an assistant professor of orthopedic surgery at Vanderbilt University Medical Center in Nashville. “This is a major issue that costs a lot of money, and no one’s done anything about it.”
The research is scheduled to be presented Thursday at the American Academy of Orthopaedic Surgeons (AAOS) annual meeting, in San Francisco.
Of the 2,000 orthopedic surgeons chosen randomly from the AAOS registry to participate in the web-based survey, 61 percent responded. Of those 1,214 surgeons, 96 percent reported they had practiced defensive medicine by ordering scans, laboratory tests, specialist referrals or hospital admissions mainly to avoid possible malpractice claims. On average, 24 percent of all ordered tests were for defensive reasons.
Using the American Medical Association’s billing codes as a reference point for costs, researchers determined that orthopedic surgeons spent nearly $8,500 per month — nearly a quarter of their total practice costs — on defensive medicine, adding up to an average of nearly $102,000 per doctor each year. Given the 20,400 practicing orthopedic surgeons in the United States, this amounts to $173 million per month and $2 billion annually nationwide, the study said.
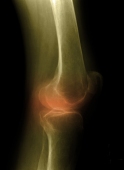
Typical scenarios resulting in unnecessary costs include patients with minor injuries who ask for MRIs after their doctors lay out a course of action that doesn’t require such a high-level diagnostic tool, physicians said. Depending on the region of the country, MRIs cost $1,000 or more per scan, Sethi said.
“It’s so ingrained in how we practice now,” said Dr. Douglas Lundy, an orthopedic surgeon in Atlanta and chair of the AAOS medical liability committee. “There’s so much faith in technology that not using it almost makes you look like you’re not doing all you can do. Also, the overall attitude of our culture is that we get everything we want pretty much when we want it.”
Researchers also found that between 70 percent and 84 percent of orthopedic surgeons who responded also practice “negative defensive medicine” by avoiding high-risk patients or procedures to limit liability. Other examples of defensive medicine include closing a practice to become a consultant, no longer seeing patients in the emergency room and not operating on patients with diabetes or heart problems.
Fixing the problem would require “massive medical liability reform at a federal level,” Lundy said, while Sethi suggested the implementation of clinical practice guidelines that would lay out treatment steps for different conditions and exonerate doctors from liability if patients develop problems outside the scope of those guidelines.
“I’m optimistic,” Sethi said. “I think physicians as a whole need to begin the steer the future of our country. I think we have to make this an issue and cut costs anywhere we can.”
More information
The Kaiser Family Foundation has more about how U.S. health care dollars are spent.

