TUESDAY, Aug. 2 (HealthDay News) — Special bioengineered spinal discs seem to grow and replace damaged discs — at least in rats, a new study shows.
While trials in humans remain years away, implants like these, made of cells and collagen, may one day help people with back pain caused by degenerative disc disease.
They might also last longer than the more artificial replacement discs in use today.
“These living implants are stiffer and stronger at six months than when we first put them in and, ultimately, they will last longer than purely metallic or plastic implants,” said study author Lawrence J. Bonassar, an associate professor of biomedical engineering at Cornell University in Ithaca, N.Y.
The new findings appear in the Aug. 1 issue of the Proceedings of the National Academy of Sciences.
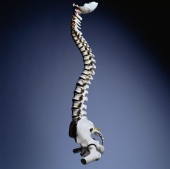
The new spinal bio-discs are composed of sheep cells in a gelatinous core, surrounded by a ring made of the protein collagen. Metal implants have traditionally been used to replace damaged discs, but they often degrade over time. The new bio-discs may have longevity on their side.
When the new discs were implanted into the spine of rats, just under the tail, they fit within the space originally occupied by the degenerated disc. After six months, the scientists used MRI and CT scans to verify that the new bio-discs had become one with the spine, and functioned much as their predecessors.
The next step, Bonassar said, is to look at these bio-discs in certain dog breeds that are known to develop degenerative disc disease, such as dachshunds and beagles, he said.
Much of the pain associated with slipped or ruptured discs is due to improper mechanical function, he noted. “If we clear out the diseased disc and the offending material and implant the new bio-disc to restore mobility, this should also relieve pain,” he said.
Study co-author Dr. Roger Hartl, an associate professor of neurosurgery at Weill Cornell Medical College and chief of spinal surgery at New York-Presbyterian Hospital/Weill Cornell Medical Center in New York City, said that treating degenerative disc disease is extremely difficult. “If we implant a metal disc, there are concerns about the longevity of the implant and the possibility of negatively affecting the levels above and below the new disc,” he said.
However, “the bio-implant over time integrates itself with the normal anatomy without negatively affecting levels above and below it,” he said. “This is the greatest advantage.”
Even though the technology is more than five years away from human trials, this latest advance “really opens up avenues of more biological treatments using tissue engineering and biologic technology to treat underlying disease processes,” Hartl said.
Still, outside experts cautioned that this concept is in its infancy and — as usual in medical science — it is a big leap to say that if it works in rats, it will work in humans.
“This is an intriguing idea, but it is a long way off from practical reality,” said Dr. Douglas Orr, a staff physician in the Center for Spine Health in the Cleveland Clinic’s Neurological Institute in Ohio. For example, while the tail of a rat does resemble the human spine, it doesn’t bear weight in the same manner, which could be an important factor.
What’s more, “only a small percentage of back pain is solely due to disc degeneration,” Orr said. Physical therapy and conditioning programs that help the back muscles compensate for the degenerative disc and/or medications are often the first line of treatment for degenerative disc disease, he said.
More information
There’s more on degenerative disc disease at the American Academy of Orthopaedic Surgeons.

