THURSDAY, April 29 (HealthDay News) — New research could change the way scientists view the causes — and potential prevention and treatment — of Alzheimer’s disease.
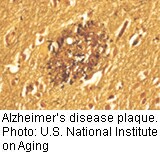
A study published online this month in the Annals of Neurology suggests that “floating” clumps of amyloid beta (abeta) proteins called oligomers could be a prime cause of the disorder, and that the better-known and more stationary amyloid-beta plaques are only a late manifestation of the disease.
“Based on these and other studies, I think that one could now fairly revise the ‘amyloid hypothesis’ to the ‘abeta oligomer hypothesis,'” said lead researcher Dr. Sam Gandy, a professor of neurology and psychiatry and associate director of the Alzheimer’s Disease Research Center at Mount Sinai School of Medicine in New York City.
The new study could herald a major shift in Alzheimer’s research, another expert said.
Maria Carrillo, senior director of medical and scientific relations at the Alzheimer’s Association, said that “we are excited about the paper. We think it has some very interesting results and has potential for moving us in another direction for future research.”
According to the Alzheimer’s Association, more than 5.3 million Americans now suffer from the neurodegenerative illness, and it is the seventh leading cause of death. There is no effective treatment for Alzheimer’s, and its origins remain unknown. For decades, research has focused on a buildup of amyloid beta plaques in the brain, but whether these deposits are a cause of the disease or merely a neutral artifact has remained unclear.
The new study looked at a lesser-known factor, the more mobile abeta oligomers that can form in brain tissue. In their research, Gandy’s team first developed mice that only form abeta oligomers in their brains, and not amyloid plaques.
Based on the results of tests gauging spatial learning and memory, these mice were found to be impaired by Alzheimer’s-like symptoms.
Next the researchers inserted a gene that would cause the mice to develop both oligomers and plaques.
Similar to the oligomer-only rodents, these mice “were still memory impaired, but no more memory impaired for having plaques superimposed on their oligomers,” Gandy said.
Another result further strengthened the notion that oligomers were the prime cause of Alzheimer’s in the mice.
“We tested the mice and they lost memory function, and when they died, we measured the oligomers in their brains,” Gandy said. “Lo and behold, the degree of memory loss was proportional to the oligomer level,” he said.
Gandy noted that PET scans are not able to detect oligomers in the human brain, but they do see amyloid plaques. This could help explain why recent trials of the experimental Alzheimer’s drug bapineuzumab showed a reduction in plaques, but no improvement in patients’ cognitive function, Gandy said.
Bapineuzumab is targeted to amyloid plaques. Whether the drug also affected the oligomers is not known, Gandy said, because the PET scans could not see them. “We don’t even know whether bapineuzumab ‘sees’ them,” he said.
The new study could help change the focus of ongoing research. “Our new ‘oligomer only’ mice may enable the development of imaging agents and drugs that lower oligomer levels without having plaques around to muddy the picture,” Gandy said.
Researchers have long been trying to figure out the stages that lead up to plaques and tangles, Carrillo noted. “We [now] know that plaques and tangles are really the end stage of this disease,” she said.
Oligomers are “toxic clumps” that could be the cause of Alzheimer’s disease, Carrillo said. This study confirms for the first time that these toxic clumps are a cause of memory problems, she said.
Carrillo noted that these results also confirm that the disease starts developing 10 to 15 years before it is diagnosed. This understanding could lead to new ways of diagnosing and treating the illness, she added.
“Perhaps future therapeutics attacking oligomers instead of plaques would be a strategy,” Carrillo said.
One expert did have some reservations about that possibility, however.
“The larger unresolved issue is how these oligomers relate to people where plaques accumulate many years prior to disease onset,” said Greg M. Cole, professor of medicine and neurology and associate director of the UCLA Alzheimer’s Center. “One would expect the little oligomer aggregates to arise prior to the bigger plaque aggregates, that is, decades before important memory problems [surface].”
That could mean that “targeting oligomers may work best for prevention,” rather than the treatment of existing disease, he said. “Ongoing efforts to track and specifically target the oligomers in clinical trials with memory deficit patients should soon tell us how much good we can do hitting the oligomers. It may be a huge success or too little, too late.”
More information
For more information on Alzheimer’s disease, visit the Alzheimer’s Association.

