WEDNESDAY, Aug. 1 (HealthDay News) — The amyloid beta protein, long tied to Alzheimer’s disease, may actually help reverse paralysis and inflammation in people with multiple sclerosis (MS).
So finds a study involving mice, conducted by researchers at Stanford University School of Medicine. While attempting to slow the progression of Alzheimer’s disease, they unexpectedly stumbled upon this promising new avenue for the treatment of MS.
“There probably is a multiple sclerosis drug in all this somewhere down the line,” study senior author Dr. Lawrence Steinman speculated in a university news release.
The study is published online Aug. 1 in the journal Science Translational Medicine.
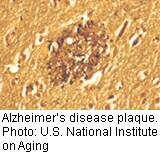
Amyloid beta is the chief component of the plaques that accumulate in the brains of people with Alzheimer’s disease. This substance builds up during the normal aging process or following a brain injury. It is also found in MS-linked brain lesions.
In conducting the study, the scientists injected amyloid beta directly into the bellies of mice with an MS-like syndrome. They report that injections delivered before the mice developed symptoms seemed to prevent or delay paralysis. The researchers added that even after symptoms appeared, the injections significantly reduced the severity of the mice’s paralysis. In some cases, they noted, the amyloid beta injections actually reversed it.
The researchers repeated their experiment to confirm their results. They concluded that amyloid beta’s influence on the paralysis and inflammation associated with MS is related to its effect on immune cells before they penetrate the brain.
“This is the first time [amyloid beta] has been shown to have anti-inflammatory properties,” Steinman noted.
After examining the central nervous systems of the mice with the MS-like syndrome, the researchers found the animals treated with amyloid beta had fewer brain and spinal cord lesions than the untreated mice. They noted there were also no increases in Alzheimer’s-like plaques in the mice treated with amyloid beta.
“We weren’t giving the mice Alzheimer’s disease” by injecting amyloid beta into their bellies, study first author Jacqueline Grant explained in the news release.
Although amyloid beta has been shown to be toxic inside the brain, its function outside the brain could be vastly different, the researchers concluded.
The protein “is made throughout our bodies all of the time. But even though it’s been studied for decades, its normal function remains to be identified,” Dr. Lennart Mucke, director of the Gladstone Institute of Neurological Disease in San Francisco and an Alzheimer’s researcher who is familiar with Steinman’s study, said in the news release. “Most intriguing, to me, is this peptide’s potential role in modulating immune activity outside the brain.”
Another expert agreed that the research has potential, but hazards remain.
“These are very impressive results that could lead to the development of new therapeutics for MS derived from the A-beta [amyloid beta] peptide,” said Philippe Marambaud, an Alzheimer’s researcher at the Feinstein Institute for Medical Research in Manhasset, N.Y.
“We have, however, to keep in mind that A-beta toxicity is not limited to the presence of plaques in the brain,” he said. “A-beta can lead to dramatic cognitive impairments in the absence of plaque formation, suggesting that the use of A-beta ‘per se’ as a potential therapeutic agent is not without risk, especially in MS patients who have a compromised blood-brain barrier.”
More information
The U.S. National Institutes of Health provides more information on multiple sclerosis.

