FRIDAY, June 14 (HealthDay News) — Older adults who get steroid injections to ease lower back and leg pain may have increased odds of suffering a spine fracture, a new study suggests.
It’s not clear, however, whether the treatment is to blame, according to experts. But they said the findings, which were published June 5 in the Journal of Bone and Joint Surgery, suggest that older patients with low bone density should be cautious about steroid injections.
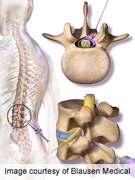
The treatment involves injecting anti-inflammatory steroids into the area of the spine where a nerve is being compressed. The source of that compression could be a herniated disc, for instance, or spinal stenosis — a condition common in older adults, in which the open spaces in the spinal column gradually narrow.
Steroid injections can bring temporary pain relief, but it’s known that steroids in general can cause bone density to decrease over time. And a recent study found that older women given steroids for spine-related pain showed a quicker rate of bone loss than other women their age.
The new findings go a step further by showing an increased fracture risk in steroid patients, said Dr. Shlomo Mandel, the lead researcher on both studies.
Still, he said, the study, which was based on medical records, had “a lot of limitations.”
“I want to be careful not to imply that people shouldn’t get these injections,” said Mandel, an orthopedic physician with the Henry Ford Health System in Detroit.
The findings are based on medical records from 3,000 Henry Ford patients who had steroid injections for spine-related pain, and another 3,000 who got other treatments. They were 66 years old, on average.
Overall, about 150 patients were later diagnosed with a vertebral fracture, Mandel said. Vertebral fractures are cracks in small bones of the spine, and in an older adult with low bone mass they can happen without any major trauma.
On average, Mandel’s team found, steroid patients were at greater risk of a vertebral fracture — with the risk climbing 21 percent with each round of injections.
The findings do not prove that the injections themselves caused the fractures, said Dr. Andrew Schoenfeld, who wrote a commentary published with the study.
But the results raise an important potential risk that needs to be weighed against the benefits. “This brings to light something that should be part of doctor-patient discussions,” said Schoenfeld, who is based at William Beaumont Army Medical Center in El Paso, Texas.
He cautioned, however, that the findings may apply only to certain patients — namely, older adults with waning bone mass. “We don’t know if this would apply to elderly people with normal bone mass,” Schoenfeld said.
Complicating matters, steroid injections seem to benefit only certain types of spine-related pain. The “best medical evidence” that they work is for cases of leg pain caused by a herniated disc compressing a nerve, Schoenfeld said.
Herniated discs are a common source of pain for younger people. “If you’re 35 and have a herniated disc, these findings don’t really apply to you at all,” Schoenfeld said.
When it comes to spinal stenosis — the most common source of problems for older adults — steroid injections can aid leg pain and cramping. But there is “very sparse” evidence that the injections ease pain concentrated in the low back, Schoenfeld said.
If that’s the primary problem for an older adult, the potential side effect of a vertebral fracture could outweigh the small chance of benefit.
Epidural steroids have been getting negative press of late. U.S. officials are currently investigating a deadly outbreak of fungal meningitis linked to epidural steroids produced by one Massachusetts pharmacy. And a study released in March found that steroid injections were less effective at relieving back pain than surgery and other treatments.
But both Schoenfeld and Mandel said the treatment still has a role in treating certain spine-related pain. They said older patients who have already found leg-pain relief from steroid injections may want to stick with them. But they should at least be aware of the potential fracture risk.
If they opt to continue the treatment, Mandel said, they may want to talk with their doctor about ways to preserve their bone mass — such as calcium and vitamin D supplements.
“There are also a number of other options for spinal stenosis,” Schoenfeld said. Normally, doctors would start conservatively, with physical therapy or medications such as nonsteroidal anti-inflammatory drugs or drugs that target nerve pain, including gabapentin (Neurontin) and pregabalin (Lyrica).
Steroid injections would be the middle ground for patients who don’t respond to those treatments but want to put off surgery, Schoenfeld said. Surgery to relieve pressure on the nerves is often effective, said Schoenfeld, although someone with spinal stenosis may later develop the narrowing in another area of spine.
More information
Learn more about spinal stenosis from the U.S. National Institute of Arthritis and Musculoskeletal and Skin Diseases.

