FRIDAY, May 24 (HealthDay News) — Patients hospitalized for heart failure appear to have better odds of survival if they’re admitted on Mondays or in the morning, a new study finds.
Death rates and length of stay are highest among heart failure patients admitted in January, on Fridays and overnight, according to the researchers, who are scheduled to present their findings Saturday in Portugal at the annual meeting of the Heart Failure Association of the European Society of Cardiology.
“The fact that patients admitted right before the weekend and in the middle of the night do worse and are in the hospital longer suggests that staffing levels may contribute to the findings,” Dr. David Kao, of the University of Colorado School of Medicine, said in a news release from the cardiology society.
“Doctors and hospitals need to be more vigilant during these higher-risk times and ensure that adequate resources are in place to cope with demand,” Kao said. “Patients should be aware that their disease is not the same over the course of the year, and they may be at higher risk during the winter. People often avoid coming into the hospital during the holidays because of family pressures and a personal desire to stay at home, but they may be putting themselves in danger.”
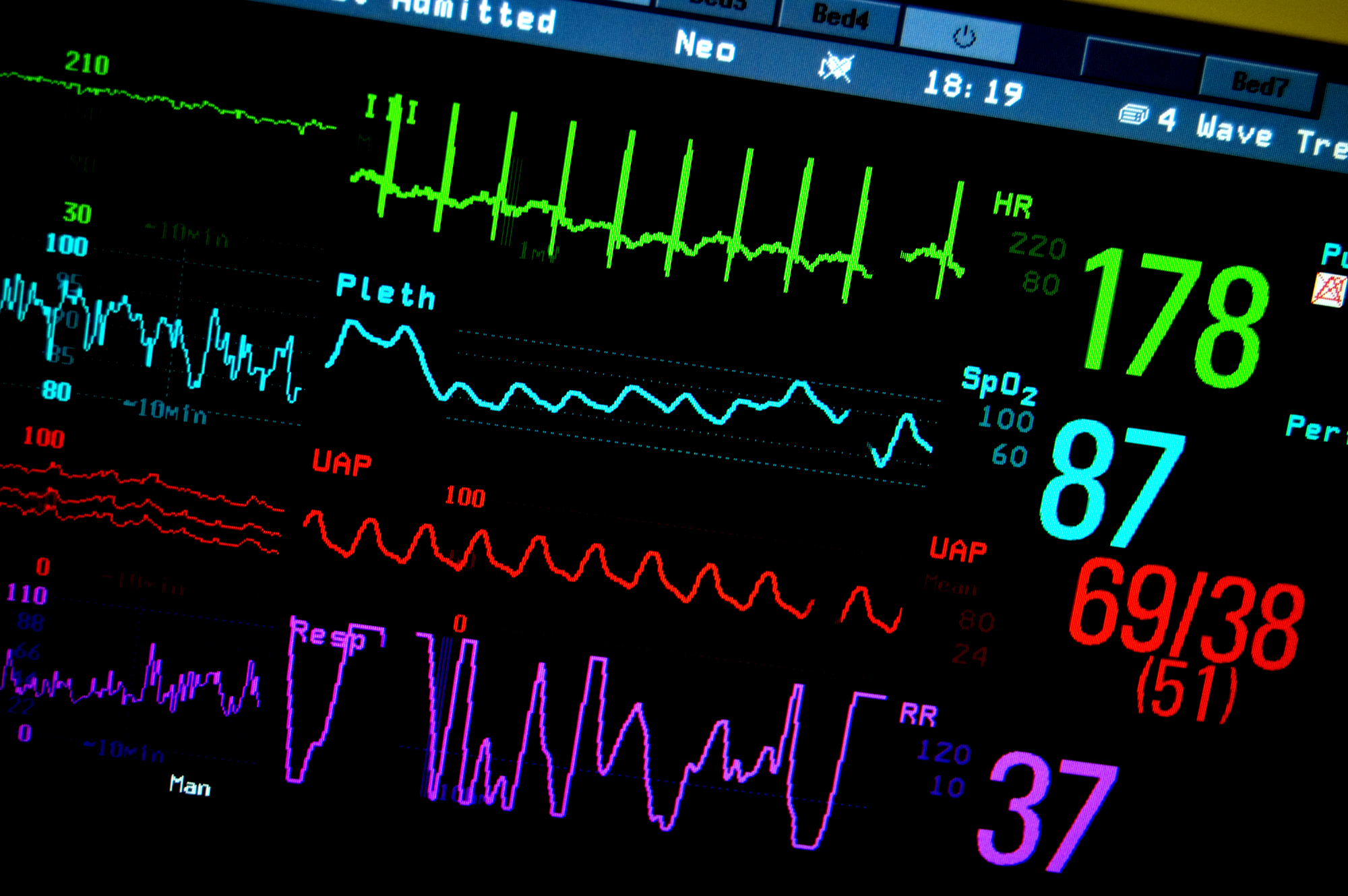
The study involved 14 years of data on more than 900,000 patients with congestive heart failure, a condition in which the heart doesn’t properly pump blood to the rest of the body. All of the patients were admitted to hospitals in New York between 1994 and 2007. The researchers analyzed the effect the hour, day and month of the patients’ admissions had on death rates and the length of time they spent in the hospital.
Patients admitted between 6 a.m. and noon fared better than evening admissions, the study found.
Although heart failure admissions have increased, the researchers found that death rates and length of hospital stays have declined. “These findings confirm the huge decline in mortality in hospitals for heart failure over the past 14 or 15 years following major advances in therapy,” Kao said.
The researchers said the seasonal spike in heart failure deaths and longer admissions was not the result of a surge in drug and alcohol abuse during the holidays, as some have suggested. “For the first time, we’ve shown that there wasn’t a higher rate of alcohol and drug use reported in heart failure patients during December and January, when heart failure mortality was the highest,” Kao said.
The researchers said greater numbers of heart failure patients who also had pneumonia during the winter could have played a role in their findings. Other respiratory illnesses, such as chronic obstructive pulmonary disease (COPD), had less seasonal variation.
“The seasonal effect on in-hospital death from heart failure remained even after controlling for time and day of admission; 17 other medical conditions, including substance use, kidney disease and pneumonia; and demographic factors, including gender, ethnicity and medical-coverage status,” Kao said. “Seasonal variations in morbidity and mortality occur in many diseases, particularly heart disease, and the cold weather itself may have a part to play.”
Data and conclusions presented at meetings typically are considered preliminary until published in a peer-reviewed medical journal.
More information
The American Heart Association provides more information on heart failure.