THURSDAY, May 9 (HealthDay News) — In the war against cancer, it looks like matchmaking — between genes and drugs — could be an important tool, according to new research into the genetic underpinnings of two rare forms of leukemia.
By matching a patient’s genetic mutation responsible for a rare, rapidly progressing form of leukemia with a drug that specifically targets the problem the mutation creates, researchers report that one patient is experiencing fast, marked improvement.
The new findings shed light on how many forms of cancer may be tackled in the near future. Scientists are discovering how to differentiate between mutations that are driving the proliferation of cancer cells and those that are merely passengers in the process.
“If your car breaks down, you have to open up the hood to see what part has broken,” said study author Jeffrey Tyner, an assistant professor at the Knight Cancer Institute at Oregon Health & Science University. “Here we have to open up the tumor cells to see what part is broken to understand what to do.”
After first identifying the genetic drivers of a specific type of cancer, scientists then match those mutant genes to drugs that will specifically target them.
According to Julia Maxson, study first author and a postdoctoral fellow at the Knight Cancer Institute, “The move in the field is to take the individual broken genes and say which of these really promote cell growth. Then, you can find the right drugs.”
The research, published May 9 in the New England Journal of Medicine, identified “driver” gene mutations related to two rare forms of blood cancers: chronic neutrophilic leukemia (CNL) and chronic myeloid leukemia (CML). The scientists identified particular mutations in the gene responsible for what is called “colony-stimulating factor 3,” which signals kinases, a type of cell enzyme.
A patient with CNL who carries that gene mutation was given ruxolitinib, a drug that specifically inhibits that mutation (and is known as a kinase inhibitor). Ruxolitinib is already on the market, used to treat a different blood cancer, called myelofibrosis. But up until now, although it has been widely available, the drug hasn’t been tried with CNL, Tyner said.
Because CNL is rare, most patients with the disease have the same mutant gene, which somewhat simplifies the process, Tyner explained. Other more common cancers will be more complicated to tackle because they are more genetically diverse, he pointed out.
“We’ll have to subdivide those common types of cancer into probably tens of thousands of subtypes of cancer, and then we’ll be able to treat them based on the drivers,” Tyner said.
The challenge is to learn which mutations are critical to causing cell proliferation, co-author Maxson explained. “We’re working to try to understand which of the mutations drive the cancer and which are just passengers in the car,” she said.
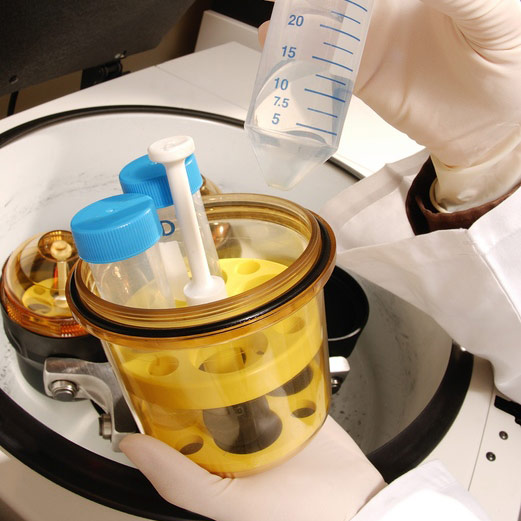
For the research, the scientists started by drawing blood from 27 patients with CNL or atypical CML, as well as from patients with other types of blood cancers. They then performed deep gene sequencing, looking at nearly 1,900 genes representing a wide range of possible culprits in cells, including kinases, phosphatases (another type of enzyme) and cytokine receptors (cells that receive messages), among others.
Then, white blood cells were distributed into thousands of different chambers, with each chamber containing a different drug or drug concentration, Maxson explained. The concept is much like how cultures of bacteria are tested against different antibiotics to see which drug works best in combating the microbes.
The researchers selected drugs that were either already approved by the U.S. Food and Drug Administration or were being tested in clinical trials. “We chose drugs that fall into the category of attacking pathways that are very likely to be uniquely sensitive on cancer cells, which is called targeted therapy,” Maxson said.
Cells were incubated for three days and then were assessed to see whether they were dead or alive — or something in between — and that showed which drugs were effective, she said. The scientists then merged the sequencing data with the drug sensitivity information.
“Genetic data helps us understand why a drug is effective, and the drug data helps us prioritize the genomic information, to know if the effect will apply to a lot of patients or to an individual patient,” Tyner said.
Dr. Jerald Radich, a member of the clinical research division at the Fred Hutchinson Cancer Research Center in Seattle, wrote in an editorial accompanying the research that “the study provides an example of the future of target discovery in cancer.”
In an interview, Radich said that “in five to 10 years, scientists will be able to assess what the best possible fits are between your tumor and the drugs that are out there.” Already, the U.S. National Cancer Institute is trying put people into specific clinical trials based on their genetic profiles, he added.
The research may be especially helpful for those who don’t respond to traditional therapy. “What we now describe as good luck or bad luck is genetics that we don’t understand,” Radich said. “We’ll look at those who completely fail regular therapy, and we’ll do whole genome sequencing — probably each patient will have 400,000 pieces of data — and from that we’ll put together a sense of what drives the genetics of nonresponders.”
For study author Tyner, the research is just the beginning. “While this study is a nice advance, it’s certainly not the end,” he said. “We’re ramping up to apply this paradigm to as many patients as we possibly can.”
More information
Learn more about leukemia from the U.S. Centers for Disease Control and Prevention.