TUESDAY, May 7 (HealthDay News) — By slowing down the programmed response rate on implantable cardioverter defibrillators (ICDs), doctors can reduce the number of shocks these devices deliver without causing a significant increase in the risk of fainting or death, new research suggests.
“The aim of [our] study was to evaluate a different programming strategy to reduce unnecessary therapies delivered by the ICD,” explained study author Dr. Maurizio Gasparini, chief of the pacing and electrophysiology unit at the Humanitas Clinical and Research Center in Rozzano, Italy.
“The study found that the strategy utilizing a long detection period to recognize arrhythmias [irregular heartbeats] is associated not only to an overall reduction of therapies, but also to less inappropriate shocks experienced by the patients as well as fewer hospitalizations in the 12 months following ICD implant,” Gasparini said.
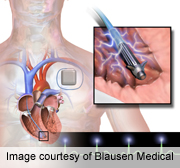
ICDs are small devices implanted in the upper chest. Electrodes from the device are attached to the heart. If an ICD senses a dangerous heartbeat or no heartbeat, it can help correct that through electrical pacing — like a pacemaker — or it can deliver a shock to the heart to restore a normal heartbeat, according to the U.S. National Heart, Lung, and Blood Institute.
Results of the study are published in the May 8 issue of the Journal of the American Medical Association. The study was funded by Medtronic Inc., which makes ICDs.
While ICDs can literally be lifesavers, they can also cause problems for some patients.
“Defibrillator shocks, whether for appropriate or inappropriate indications, are associated with adverse effects. These adverse effects include the acute discomfort of the shock, as well as late and longer-lasting psychological trauma including depression and post-traumatic stress disorder,” wrote Dr. Merritt Raitt, author of an accompanying journal editorial. Raitt is with the Oregon Health and Science University and the Portland Veterans Administration Medical Center, in Oregon.
The current study included about 1,900 people who were receiving their first ICD implant. Their average age was 65, and 84 percent of the study volunteers were male.
The volunteers were randomly placed into one of two groups: standard programming or programming with a long detection interval.
“Every time the heart beats, an electrical activity is recorded by the device. An interval is the time between two consecutives beats. Basically it is the time between two heartbeats. So, a long detection interval simply means a longer period of time to permit recognition of arrhythmias,” Gasparini explained.
During an average of 12 months of follow-up, 530 episodes of an arrhythmia were recorded. The long detection group had a 37 percent lower rate of delivered therapies (pacing or shocks) than the standard therapy group, according to the study.
There were no significant differences in mortality or in fainting (syncope) episodes between the groups.
“This study shows that we can decrease inappropriate and unnecessary therapies, and clearly you make people feel better because they’re not getting inappropriate or unnecessary therapy, said Dr. Ranjit Suri, director of the electrophysiology service and Cardiac Arrhythmia Center at Lenox Hill Hospital in New York City.
However, Suri said it’s not yet clear what the ideal interval time is. The current study doesn’t show a benefit in terms of reduced risk of death. Another study, published last December in the New England Journal of Medicine, did find a mortality benefit. But, the interval was longer in that study.
Still, Suri said, doctors could start programming ICDs with longer intervals, and making such a change to the device isn’t difficult or time-consuming.
In his editorial, Raitt wrote: “Regardless of whether these programming interventions lead to reduced mortality, the unequivocal reduction in ICD shocks and the reduction in hospitalization without an increase in adverse events such as syncope suggests that this programming approach should be considered for adoption in the care of patients with ICDs and clinical characteristics similar to those enrolled in these studies.”
Study author Gasparini noted that the research provides physicians with an easy programming guideline that’s “applicable to the great majority of patients who may benefit from the reduction of unnecessary painful shocks and hospitalizations.”
More information
Learn more about implantable cardioverter defibrillator from the U.S. National Heart, Lung, and Blood Institute.

