MONDAY, Feb. 28 (HealthDay News) — A new study adds more weight to research showing the risk of developing Alzheimer’s disease is greater if your mother, rather than your father, had the disorder.
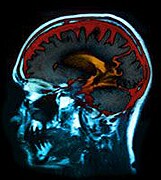
Brain scans of adult children of people with Alzheimer’s found more shrinkage in key brain regions of those whose mothers had the disease than in those whose fathers had it, the researchers report. Brain shrinkage is a characteristic of the age-related disorder.
“It’s consistent with other studies that suggest there is something inherited from mothers that influences risk more so than what is passed down through fathers,” said senior study author Dr. Jeffrey Burns, an associate professor of neurology at University of Kansas Medical Center.
Alzheimer’s disease has a strong inherited component, according to background information in the study. Those whose parents had the disease are four to 10 times more likely to get the disease themselves.
In the study, researchers created three-dimensional maps, using a technology called voxel-based morphometry, of the brains of 53 people aged 60 and older. Eleven had a mother with Alzheimer’s, 10 had a father with Alzheimer’s and the rest had no family history of the disease.
None of the participants had dementia when they were recruited, nor did they show the signs of mental decline that can be an early indicator of the disease, researchers said.
After two years, people whose mothers had Alzheimer’s had twice the amount of gray matter atrophy, or shrinkage, in brain regions known to be affected by Alzheimer’s compared to those with a paternal history or no family history of the disease. The regions included the parahippocampal gyrus and the precuneus.
Those with a maternal history of Alzheimer’s also had one and a half times more loss in whole brain volume each year compared to those with a paternal history or no family history of the disease.
The study is published in the March 1 issue of Neurology.
A small amount of brain shrinkage with each passing year is common among older adults and not necessarily a sign of Alzheimer’s, Burns noted.
However, with Alzheimer’s, the atrophy occurs much faster.
Researchers don’t know what the Alzheimer’s-related inheritance from mothers is, but they theorize that it may have something to do with mitochondrial dysfunction. Mitochondria, which generate the energy that cells use to function, are inherited only from mothers.
Prior research has linked mitochondrial problems and Alzheimer’s disease, Burns said.
“This suggests that the mitochondrial dysfunction may have more to do with Alzheimer’s than we previously have considered,” he said.
Dr. Steven DeKosky, a professor of neurology at University of Virginia School of Medicine, said too few participants were involved in the study to draw a conclusion. Larger studies are needed to confirm the findings, he said. In addition, researchers did not test for specific proteins associated with Alzheimer’s, such as those found in cerebrospinal fluid.
Testing for those protein markers could confirm if the atrophy was indeed due to Alzheimer’s, DeKosky said.
“I would be very cautious about reaching any firm conclusions about genetics from this study,” DeKosky said.
“They probably have identified AD [Alzheimer’s disease] cases which are presymptomatic, but whether the male-female difference will be maintained would await larger numbers of cases, perhaps more thoroughly characterized,” he added.
With Americans living longer, cases of Alzheimer’s disease are soaring in the United States. By 2030, about 20 percent of the total U.S. population will likely have the disorder, the Alzheimer’s Association estimates.
More information
The U.S. National Institute on Aging has more on Alzheimer’s.

