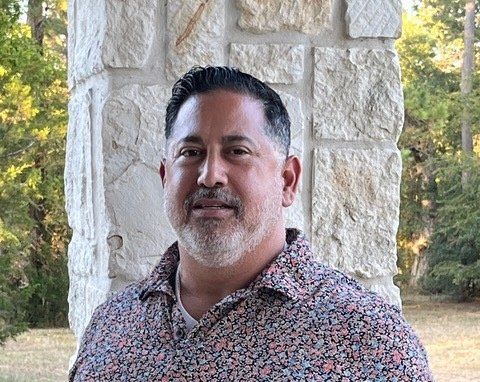
MONDAY, May 1, 2023 (HealthDay News) — Hito Bazan never knew how much he’d appreciate every breath he takes until one day he couldn’t do it.
The Houston police officer awoke one morning not able to eat, walk, talk or even breathe after three months in the hospital with COVID-19 and double pneumonia.
That was back in 2020, and the now-retired Bazan was soon diagnosed with an interstitial lung disease (ILD) known as pulmonary fibrosis (PF).
“Two years ago, the quote ‘breathing is the greatest pleasure in life’ wouldn’t have meant much to me. Today, it means everything,” Bazan said. “With each breath, I’m determined not to let this disease keep me down. I’m going to continue living my life the best I can.”
When COVID was new, it wasn’t known exactly where it would lead in terms of human health and long-term effects. Those effects are now becoming clearer more than three years after the new coronavirus began spreading around the world.
The Pulmonary Fibrosis Foundation (PFF) shares what it knows about post-COVID ILD, how it occurs and the available treatments.
“There weren’t a lot of answers in the beginning,” Bazan said in a foundation news release. “I’ve come a long way since then, and we know a lot more about post-COVID ILD than we did nearly three years ago.”
In PF and ILD, scarring appears in lung tissue. As this scar tissue builds up over time and blocks the movement of oxygen from the lungs into the bloodstream, these low oxygen levels can make someone feel short of breath. This is particularly true when they’re exerting themselves, such as when walking and exercising.
The symptoms someone experiences with ILD after COVID can be similar to those experienced by those with ILD not caused by COVID. They include shortness of breath, fatigue and a chronic, dry cough.
Some people feel worse over time, while others have gradual improvement in their symptoms or stable but persistent cases. People with ILD after COVID-19 may also have symptoms of long COVID, such as heart palpitations, chest pain or difficulty thinking and concentrating.
“The symptoms of shortness of breath and cough are common to many different illnesses, so if one has these symptoms following a COVID-19 infection, it does not always mean that ILD is present,” said Dr. Amy Hajari Case, senior medical adviser for education and awareness for the PFF. “Persistent symptoms should always prompt a conversation with your medical provider.”
Bazan’s COVID pneumonia put him at risk of developing PF and ILD. Having severe COVID, especially with acute respiratory distress syndrome (ARDS) and mechanical ventilation, are also risk factors for the condition. Sometimes ARDS can lead to permanent lung damage.
“The impact of the COVID-19 pandemic has been unprecedented. We are still learning the ways in which post-COVID ILD affects patients and continue to gain a better understanding of the progression of the disease for patients with different risk factors and exposures,” Hajari Case said in the release. “In time, we are hopeful that more research will emerge to shed light on the causes of post-COVID ILD and the long-term effects on our overall health.”
Doctors can diagnose post-COVID ILD using chest imaging, analyzing a patient’s persistent respiratory symptoms, doing blood work and having the patient undergo pulmonary function tests that measure the amount of air the lungs can hold. A high-resolution computed tomography (HRCT) scan can reveal detailed images of the lung.
Sometimes a diagnosis may require a lung biopsy.
Treatment can vary because guidelines don’t exist yet. A doctor may monitor the patient’s disease or prescribe steroids, including prednisone, if there is lung inflammation.
In the meantime, anti-fibrotic medications pirfenidone and nintedanib are now being studied in clinical trials of ILD after COVID-19.
“While there is significant uncertainty regarding the prognosis of ILD after COVID-19, studies show that most survivors of severe illness from COVID-19 experience gradual improvement or stability, although they may have ongoing lung function impairment if they developed PF,” Hajari Case said. “Studies are essential to better understand the natural history and risk factors for development of ILD after COVID-19.”
The organization notes that pulmonary rehabilitation, supplemental oxygen, smoking cessation, routine vaccinations and disease management by a skilled specialist can help patients with ILD have an improved quality of life.
Bazan had to retire after his PF diagnosis, but finds that with an oxygen machine and the right medical care he is still able to exercise, complete DIY projects around his house and spend time with his family.
“It was a long road getting back to where I am now,” Bazan said. “I used to be very focused on work, but now I’m driven to beat this disease, and I’m not going to stop living. I’ve learned that life does not end — it just takes some adjustments.”
More information
The U.S. Centers for Disease Control and Prevention offers more on post-COVID conditions.
SOURCE: Pulmonary Fibrosis Foundation, news release, April 27, 2023
Copyright © 2026 HealthDay. All rights reserved.