TUESDAY, March 21, 2023 (HealthDay News) — The hit HBO series “The Last of Us” portrays a zombie apocalypse caused by a fungal infection that hijacks human brains.
Back in the real world, there’s an emerging fungal threat rampaging through the United States, a new study warns — one that doesn’t turn humans into zombies, but does endanger lives.
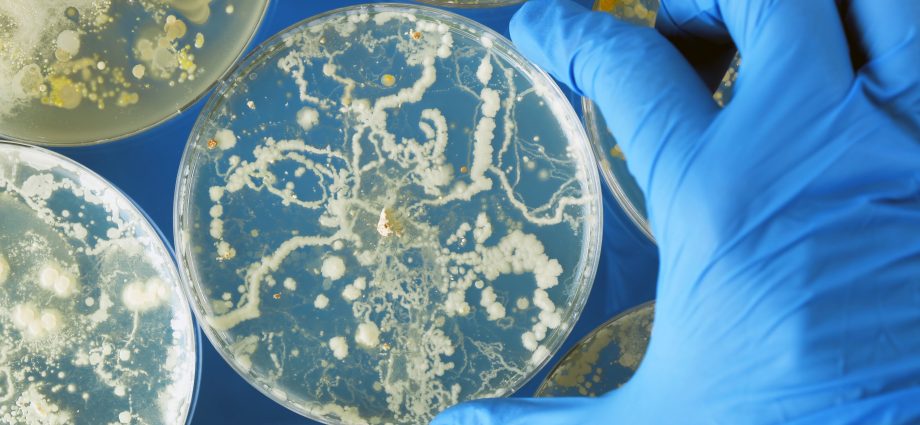
Candida auris has surged across the nation since the first case occurred in 2013, researchers from the U.S. Centers for Disease Control and Prevention reported in the March 20 issue of the Annals of Internal Medicine.
The yeast easily spreads through touch, is difficult to clean away, and can remain viable on surfaces for months, noted lead researcher Dr. Meghan Lyman, a medical officer in the CDC’s Mycotic Diseases Branch.
While it’s innocuous to healthy people, C. auris can cause severe and life-threatening infections in people whose immune systems have been compromised by other illnesses.
The percentage of dangerous infections caused by C. auris has increased every year in the United States, from a 44% increase in 2019 to a 95% increase in 2021, the new study found.
More than one in three patients with an invasive C. auris infection — for example, an infection of the blood, heart or brain — die, according to the CDC.
C. auris has now been reported in 28 states and the District of Columbia as of 2021, up from just four states in 2016, the researchers reported.
“We’ve been seeing a steady increase, and the increase has gotten more dramatic in more recent years,” Lyman said.
Not only is C. auris spreading to more states, but there are more cases occurring in the states where the fungus has gained a foothold, Lyman said.
There’s also been a drastic increase in the number of people who have been colonized with C. auris and carry it around, potentially spreading the fungus to others.
There was a 209% increase in cases of healthy people who screened positive with C. auris in 2021, compared with a 21% increase the year before, the researchers found.
Worse, C. auris is increasingly resistant to antifungals, Lyman said.
There are three classes of antifungal medicines, and the yeast started out as often resistant to two out of the three, Lyman said.
But C. auris is now developing resistance against the third line of defense, a newer semi-synthetic class of antifungal called echinocandins, the investigators found.
The number of C. auris cases resistant to echinocandins in 2021 was about three times that of cases identified in each of the previous two years, the new study showed.
“That’s the first-line treatment for C. auris, as well as other invasive Candida infections,” Lyman said. “The number of resistant cases in the U.S. is still low, but we’re seeing an increase and that’s definitely concerning to us because the treatment options for those patients would be more limited.”
C. auris was first detected in Japan in 2009, Lyman said. It was isolated from a patient’s ear — “auris” is Latin for “ear.”
The first U.S. case occurred in 2013 but was not identified and reported until 2016, the study authors said.
There are several different strains of C. auris circulating in the United States, leading researchers to believe that it was introduced from abroad several different times by patients who were colonized in other countries, Lyman said.
Some theories hold that climate change has contributed to the rise of this fungus, Lyman said.
“Candida auris actually likes to grow in slightly hotter temperatures than other species,” Lyman said.
Another theory holds that overuse of antimicrobial agents is partially responsible, by killing off other fungal species and allowing the more resistant C. auris to propagate, Lyman said.
“But I think the more recent spread in the U.S. is really related to poor infection control practices in these health care settings,” Lyman said.
C. auris is easily transmitted through touch, and can spread rapidly through nursing homes, long-term care facilities and hospitals, Lyman explained.
“It sheds from people into the environment and contaminates surfaces like beds or tables, and also mobile medical equipment that can go from patient to patient or even health care workers,” Lyman said.
One of the very first outbreaks reported in the United Kingdom involved thermometers that were being placed in people’s armpits to take their temperature, Lyman said.
“They were cleaning the devices, but what they were using wasn’t working,” Lyman said. “A lot of work is being done to identify disinfectants that do work, and now there’s a list of disinfectants that have been tested and approved for use against Candida auris.”
Unfortunately, C. auris spreads so quickly that by the time the first severe infection occurs, many people have become colonized with the yeast.
“You find this case and then when you start screening, you find that it was introduced quite a while ago and it’s been circulating for some time on patients who are colonized but without clinical specimens,” Lyman said. “There’s already been quite a bit of spread by the time you detect the problem.”
Many hospitals have taken to regularly screening patients for C. auris who are arriving from nursing homes, long-term care facilities and other places known to have active spread of the fungus, said Dr. Aaron Glatt, chief of infectious diseases and a hospital epidemiologist with Mount Sinai South Nassau in Oceanside, N.Y.
Doctors now are struggling to decide what to do with patients who are colonized with C. auris but are not infected, Glatt said.
“If you are colonized, we don’t recommend treatment. We recommend good infection control,” Glatt said. “You don’t want to create further resistance by inappropriately using antifungals. There’s no reason to treat a colonized person. You don’t want to worsen things by treating inappropriately.”
But this approach threatens to create a caste of medical outcasts, Glatt said — people colonized with C. auris who find themselves isolated from other patients and ostracized from long-term care facilities.
“There’s consequences of being identified as having Candida auris,” Glatt explained. “Nursing homes don’t want to take these patients. They’re languishing in hospitals. You screen and identify them, and then these people become pariahs.”
However, early identification of people carrying C. auris, along with better infection control and new antifungal medications, is one of the best ways to ward off future spread, Lyman contends.
“A lot of the approaches have been very reactive — once you see it’s a problem, then you try and implement changes,” Lyman said. “What would be best is to be more proactive, really looking for it and screening to try and identify colonized individuals early so they can be put on precautions to prevent spread.”
Even though her report seems dire, Lyman said early attempts to contain specific C. auris outbreaks show there is hope.
“There have been facilities in areas that have seen success with preventing spread or containing an outbreak. There have been some facilities that have had big outbreaks, and obviously it took a lot of work, but they were able to control the situation and stop spread,” Lyman said. “We don’t want people to be hopeless and feel like this is inevitable. There’s a lot that can be done to stop the number of cases and prevent the dramatic increase that we’ve been seeing.”
More information
The U.S. Centers for Disease Control and Prevention has more about Candida auris.
SOURCES: Meghan Lyman, MD, medical officer, mycotic diseases branch, U.S. Centers for the Disease Control and Prevention; Aaron Glatt, MD, chief, infectious diseases, and hospital epidemiologist, Mount Sinai South Nassau, Oceanside, N.Y.; Annals of Internal Medicine, March 20, 2023
Copyright © 2026 HealthDay. All rights reserved.